Changes over time in how autism is defined as well as improved access to diagnosis are the most likely reasons why autism diagnoses have jumped in recent years, according to Harvard T.H. Chan School of Public Health’s Ari Ne’eman.
Ne’eman, assistant professor of health policy and management and an expert on autism and disability policy, shed light on the issue in a Sept. 30 opinion piece for STAT, written in the wake of Health and Human Services Secretary Robert F. Kennedy Jr.’s assertion that there is an autism “epidemic.”
According to the most recent CDC estimate, one in 31 eight-year-old children in the U.S. had autism spectrum disorder in 2022, up from one in 150 in 2000. But Ne’eman pointed out that changes in how mental disabilities were diagnosed have played a big role in that increase. Decades ago, he wrote, many people who would today be diagnosed with autism received other diagnoses, such as “intellectual disability.” But as researchers learned more about such disabilities, many individuals were shifted into other categories—notably, autism—as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM), a handbook published by the American Psychiatric Association that provides a common language for diagnosing mental health conditions.
Ne’eman also noted that, as autism diagnoses have increased in recent years, there have been corresponding declines in other diagnoses, such as “intellectual disability” and “learning disability”—which suggests “that a process of diagnostic substitution was taking place rather than a real increase in autism prevalence,” he wrote.
Another factor in the increase in autism prevalence has been improved access to diagnosis, particularly among racial and ethnic minority groups and among households of lower socioeconomic status, according to Ne’eman.
In addition to mischaracterizing the prevalence of autism, the Trump administration is making matters worse with plans to cut federal funds and programs that support people with autism and other disabilities, he added.
Read Ne’eman’s STAT article: The Trump administration’s Soviet approach to autism policy
Learn more
A research agenda to improve the lives of autistic people (Harvard Chan School news)
Last Updated
Featured in this article
CAUSALab Announces the 20th Kolokotrones Symposium

CAUSALab announced the 20th Kolokotrones Symposium this week.
“Acetaminophen During Pregnancy and Autism: What Does Causal Inference Take?”
The fall symposium will be held November 14, 2025 (1:30-3:30 PM ET) and provide an introduction to the epidemiology of autism, present what is currently known about the association of acetaminophen use during pregnancy and autism, describe possible explanations for this association, and explore the challenges and opportunities to design better studies to estimate the causal effect. The symposium will conclude with an expert panel that will consider the question: where do we go from here?
Speakers & panelists: Marc Weisskopf (NIEHS Center for Environmental Health, Harvard T.H. Chan School of Public Health), Krista Huybrechts (H4P, Harvard T.H. Chan School of Public Health), Brian Lee (Drexel University Dornsife School of Public Health), Sonia Hernández-Díaz (CAUSALab, H4P, Harvard T.H. Chan School of Public Health), Alec Walker (Harvard T.H. Chan School of Public Health) – Moderator
In-person attendance is limited to Harvard ID holders due to space restrictions. Online attendance is free and open to the public. Speakers’ remarks are based on their own scholarship and experience. As such, they speak for themselves, and not for Harvard University.
Registration is open now on Eventbrite.
Last Updated
MPH Generalist student makes case for the ethics of health equity programs

Alan Hernandez Gutierrez, MPH ’26, manages a health clinic while taking classes and just had his first paper published.
Alan Hernandez Gutierrez never expected that the first article he’d ever written would get published, much less on the first try. He’d drafted “Ethics of advancing racial health equity in public health” for a course, drawing on his personal background and experiences as a health clinic manager in the San Francisco Bay area. The paper looked at the Abundant Birth Project, a pilot guaranteed income program for Black and Pacific Islander mothers—one of several guaranteed income programs launched by the city to tackle disparities among specific groups, and the only one that has not yet been terminated following anti-discrimination litigation.
Hernandez Gutierrez argued that the idea that health equity programs are discriminatory is misguided, and that initiatives such as the Abundant Birth Project are not just ethical but “obligatory if we are to shape a society that ensures all have equal rights to health and dignity.”
His ethics instructor Susannah Rose encouraged him to see if he could get the paper published or present it at a conference. After giving it an additional polish over the summer, he wrote up a list of potential journals and submitted it to the first one on his list, the Oxford Journal of Public Health. To his surprise, it was accepted and published in September.
His practicum advisor Bill Bean is thrilled for Hernandez Gutierrez and enjoys taking the opportunity to brag about him. “In working with Alan, there is a real sense of joy that he has in learning new things and opening himself up to the possibilities of public health,” he said. “His optimism and excitement are palpable.”
Hernandez Gutierrez recently spoke about why he advocates for racial health equity and his path into public health.
Q: Why did you choose to write about the ethics of advancing racial health equity in public health?
A: I watched what was happening with San Francisco’s guaranteed income pilot programs. People who were challenging these programs in court were using language around equity and inclusion and calling them discriminatory because they focused on helping certain groups. It really rubbed me the wrong way to see the type of language that had been used to uplift me and my community as a young gay man now being used in legal arguments against these programs.
In my work as a health clinic manager, I’ve been involved with health equity initiatives for years. It’s always felt like a very normal bread-and-butter aspect of our work to prioritize finding ways to help the most impacted folks. Seeing these court cases, where health equity was viewed through a lens where it wasn’t considered ethical, led me to want to dig in and try to understand what was going on.
In this country, people like to blame individuals for their “poor choices.” But there is a larger system impacting not just the choices people make but whether they even have a choice available. Two people with identical aspirations or goals can have distinctly different outcomes in spite of having the same personal motivation, due to both their access to resources and how they are valued in society—both of which are arbitrary. I believe that when you help those who are most impacted, ultimately, you end up removing barriers for everyone.

Q: What was your path into public health?
A: It started with archaeology—which was an obsession when I was a kid. That led me to anthropology, which was one of my undergraduate majors at the University of California, Berkeley. I took a couple of medical anthropology courses, and one of them delved into medical racism and the history of race. I got really interested in the subject and what it looks like in modern society, so going into health care and public health after I graduated made a lot of sense to me.
I really wanted to have some sort of impact, so I joined a federally qualified health center, the Haight-Ashbury Free Clinic in San Francisco. I started off at the front desk, primarily registering patients. But within a couple of months, I was able to move into a manager position, and my career took off from there.
At the practices where I’ve worked, I’ve been able to design innovative and interesting interventions to tackle specific issues that we see with our patient populations. For example, at the Haight-Ashbury Free Clinic, I worked on substance abuse screening in our dental clinic, getting folks looped into our addiction services in the primary care clinic. Now that I’m a clinic manager at Stanford Health Care, the patient population I serve is very different, but the job is still a lot about project design and meeting needs.
I currently manage the endocrinology and internal medicine clinics, in addition to an express care clinic that we opened over the summer. It is essentially a middle area between primary and urgent care and has been a way to increase timely access for our current patients and people who might not already have a history with us. As my practicum for my MPH degree, I worked with other members of my team to design the express care clinic, which involved, for example, thinking about what types of patients we’re going to see and what resources we’d need.
Q: Why did you decide to pursue an MPH Generalist degree?
A: I had always planned to go to graduate school and earn a PhD, but I felt burned out after my bachelor’s degree and wasn’t sure where to go. As I continued working in public health and health care, it became clear that it’s something I really love and am passionate about. I wasn’t ready to commit to a PhD, but this program allowed me to test the waters.
Throughout my professional experience, I’ve learned a lot about the social determinants of health and health equity. But I really wanted an academic foundation in these concepts and how to apply them.
Q: How has your experience been so far?
A: It’s been really great. I cannot imagine a better program to have been in. The staff are supportive, and the faculty have been amazing. I mainly complete my work in the evenings and on the weekends, but whenever there’s an opportunity for a live session, I love to jump on. I also took advantage of the optional in-person summer session.
I message a few faculty in the program frequently like Bill Bean. I feel so much at home with Harvard Chan School, even though it’s remote. I feel like the program does a great job at cultivating a community, not just with the other generalist students, but with the staff and faculty.
Q: What are your career goals after you finish your degree?
A: I’m at a fork in a road. I would love to do a PhD around health policy or medical anthropology. At the same time, I really love the work I’m doing in public health and health care. I get to see a lot of what’s going on in people’s lives day to day, and I feel like sometimes with academia, it’s possible to have a little too much separation. If I continue working in health care and public health administration, I would love to design interventions with a larger scope beyond my clinic. If I decide to focus on academia, I’d love to go into health policy.
Q: What keeps you motivated to work in public health?
A: It really excites me. The world can feel hopeless right now, but public health imagines what a better future can look like. It’s helped me understand that we have the resources and the know-how to make change—it’s really just about finding the political will to actually do things.
Quick hits
My favorite way to unwind is putting on my headphones and just listening to music. As I’ve gotten older, I’ve become open to any type of music that sounds good to my ears—anything from classical to Chappell Roan.
I taught myself to juggle last year. I always wanted to learn. Now I can do a very basic three-ball juggle, nothing fancy.
Circe by Madeline Miller is a book I like to recommend. It’s about working for your magic. I’ve loved Greek mythology since I was a little kid, and this book subverted how I thought about it. I think the trope of being born with a skill or power is a little boring. I like the idea that through hard work, trying and failing, you get to do something wonderful.
Last Updated
Featured in this article
Last Updated
Featured in this article
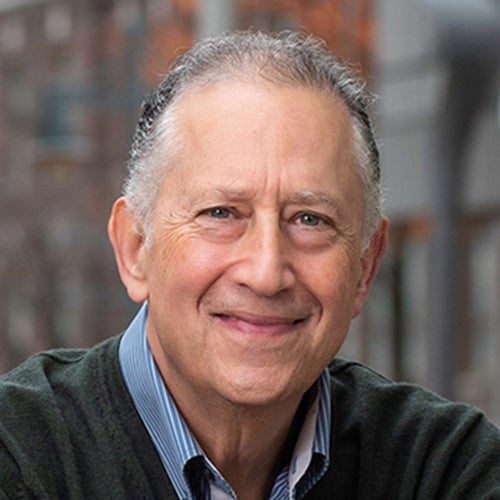
Strong social connections could boost healthy aging, experts say

Having a rich social life may do more than brighten your days—it could also help slow biological aging, according to a new study.
Co-authors of the study, published in the journal Brain, Behavior, and Immunity, included Laura Kubzansky, professor of social and behavioral sciences at Harvard T.H. Chan School of Public Health, and researchers from Cornell University, Weill Cornell Medicine, and Renaissance School of Medicine at Stony Brook University.
Drawing on data from more than 2,100 participants in the long-running Midlife in the United States (MIDUS) project, researchers discovered that adults with higher cumulative social advantage—meaning long-standing, robust relationships with family and friends and in religious and community groups—had biological markers showing slower cellular aging and reduced levels of chronic inflammation as compared to their less-connected peers.
Jeremy Nobel, instructor in the Department of Health Policy and Management, commented on the study in an Oct. 7 article in Everyday Health.
“Social circumstances, both objective and subjective, have measurable biologic change that is related both to aging and to illness,” he said. “This can allow us to compare the influence of certain external factors on the speed of aging at the cellular level, and it can also allow us to measure the impact of various interventions on aging, which is exciting for those like me who are working as public health practitioners.”
Nobel recommended prioritizing social connections alongside diet, exercise, and sleep, and suggested that people view loneliness as a fundamental biological signal, “just like thirst is a biological signal that we need hydration. Loneliness does impair our health, so it’s not surprising that we, our bodies and our minds, have generated a mechanism to tell us to go out and connect with others.”
Read the Everyday Health article: Strong Social Ties May Slow Biological Aging
Last Updated
Featured in this article
WHO director-general Dr. Tedros Adhanom Ghebreyesus receives Elisabeth B. Weintz Humanitarian Award

Dr. Tedros Adhanom Ghebreyesus, director-general of the World Health Organization (WHO), received the 2025 Elisabeth B. Weintz Humanitarian Award from the Harvard Humanitarian Initiative (HHI). The award was presented at an Oct. 8 ceremony and lecture at Harvard T.H. Chan School of Health titled “Global Health in a Fractured World.”
Dr. Tedros was recognized for his work as a global humanitarian leader and public health champion. In his remarks, he outlined his efforts to help the WHO and its member states adapt to drastic cuts in global aid funding and called on members of the Harvard Chan School community gathered in Kresge G1 for the event to join in this work.
“We need leaders and policymakers who see health not as a cost to be contained, but an investment to be nurtured in security, stability, and economic prosperity. We need scientists, researchers, and health professionals not only to do their vital work, but to communicate it with courage and clarity,” he said. “And we need citizens to raise their voices for equity and justice. Demand that your leaders invest in health, not as a privilege, but as a fundamental human right for every human being, everywhere.”
It was a return visit to campus for Dr. Tedros, who served as the School’s commencement speaker in 2021. Throughout his career, he has led global health initiatives on HIV/AIDS, malaria, and maternal and child health, coordinated international responses to threats such as Ebola, COVID-19, and mpox, advocated for universal health coverage, and worked to protect civilians in conflict zones. Prior to becoming WHO director-general in 2017, he served in the Ethiopian government as minister of health and minister of foreign affairs.
The event, co-presented by the Harvard Chan Studio, also marked the 20th anniversary of HHI, the University’s hub for advancing the science and practice of humanitarian assistance. Founding director Michael VanRooyen, Lavine Family Professor of Humanitarian Studies in the Department of Global Health and Population, spoke in his introductory remarks about the challenges currently facing public health, especially in the humanitarian sector. “It’s a time when we need strong principled leadership to help guide us, and that’s what we’re here to celebrate today,” he said.
Primary care, peace, and global solidarity

In his remarks, Dr. Tedros emphasized his deep personal commitment to addressing health inequity around the world. He recalled an early memory of walking with his mother in his hometown in Ethiopia and seeing posters about smallpox and the organization that was working to eradicate it—the WHO. He said that at the time all he knew about infectious diseases was that they could quickly cause children to be “snatched away.” His own brother died of a disease that could have been prevented, likely measles, he said.
“Inequity and insecurity were not things I read about,” he said. “They were things I saw and experienced every day. They happened to me, and they happened to my family. And inequity and insecurity continue to be the driving forces of my life and career.”
Despite advances in medicine and public health, there is currently a 31-year gap between countries with the highest and lowest life expectancies, he said. And lack of access to essential health care and adequate nutrition still cause numerous deaths around the world. “Health inequities are not natural or accidental. They are the result of systemic differences in the opportunities people get, the resources they can access, and the power they hold,” he said.
He spoke about three areas where he sees fractures in the world today: health systems, security, and solidarity, which he characterized as bilateral aid and multilateral cooperation.
But he said that despite the gravity of these fractures, his diagnosis for the world is not terminal. They can be healed through actions including strengthening primary health care, promoting peace, and supporting greater global cooperation, he said.
More global engagement, less aid
The WHO is under pressure from funding cuts by the U.S. and other countries, Dr. Tedros said. Earlier this year, member states approved a significantly reduced budget at WHO, and cost savings measures including workforce reductions have been introduced. He said that he is trying to use the current situation as an opportunity to make the WHO stronger, more independent, and focused on its core mandate to serve people around the world. These efforts include greater reliance on scientific partnerships, broadening the WHO’s donor base, and establishing an endowment.
The WHO has also learned from COVID-19, he said, and is working with member states and partners on ensuring a more coordinated response to future pandemics—for example, through establishment of an mRNA technology transfer hub and adoption of a pandemic agreement.
In addition, Dr. Tedros said that the WHO is supporting countries that are ready to transition from aid dependency to sustainable self-reliance. This work includes identifying ways to improve efficiency and generate new revenues for health from domestic resources such as sales taxes on tobacco, alcohol, and sugary drinks.
“In the end, the fractures in our world are fractures in our politics and in our collective will. But I believe it’s within our power to mend them,” he said. “We have the tools. We have the knowledge. What we need now is the courage to make the right choices—to choose solidarity over nationalism, equity over greed, and evidence over ideology.”
Support for humanitarian research and education
The Weintz Award recognizes individuals with a record of achievement and impact in the humanitarian field who have demonstrated an extraordinary contribution towards alleviating human suffering.
The award was established in 2015 by J. Frederick Weintz to celebrate his late wife Elisabeth “Betsy” Weintz. The Weintzes were early supporters of creating a program at Harvard focused on improving the humanitarian response to global crises through research and education, which, with their ongoing support, evolved into the Harvard Humanitarian Initiative.
In her introductory remarks, Marcia Castro, Andelot Professor of Demography and chair of the Department of Global Health, recognized members of the Weintz family who were in attendance. At a time when funding for global aid has been cut and public health research remains under threat, generosity like theirs is needed more than ever, she said.
Last Updated
Featured in this article
Op-ed: Ultra-processed foods should not be focus of U.S. nutrition policy

A “Make America Healthy Again” report on childhood health, released by the White House in May, cites ultra-processed food as a leading cause of chronic disease—but making these foods “the new dietary villain” could be a misstep, according to Harvard T.H. Chan School of Public Health’s David Ludwig.
In an Oct. 6 Washington Post op-ed, Ludwig, professor in the Department of Nutrition, wrote that ultra-processed foods are defined imprecisely and studies have not definitely shown that diets without them have long-term health benefits. Therefore, he argued, nutrition policies should not overgeneralize and recommend that all of them be cut out.
He recounted the major effort by the U.S. government and nutrition experts half a century ago to convince the public to follow low-fat diets in order to prevent chronic disease. However, the approach was not strongly supported by research and led to unintended consequences: Processed carbs such as sugary beverages and sweetened breakfast cereals became commonplace, and obesity and diabetes rates increased.
Ludwig pointed out that ultra-processed foods—defined as having at least one major food component or additive not used in traditional cooking methods—include actually healthy foods such as olive oil created by processing olives. Furthermore, the potential health benefits of diets without ultra-processed foods have not been studied comprehensively, he noted.
“Launching another broad public health prevention campaign based on ambiguous observational studies and weak clinical trials risks a redux of the low-fat diet debacle,” he wrote. He recommended that health officials should instead focus on the subset of foods that have strong scientific evidence of causing harm, including refined grains, sugar, and other highly processed carbohydrates.
Read the Washington Post op-ed: Dietary fat was a scapegoat. Now MAHA is naming a new one.
Last Updated
Featured in this article
Study reveals crisis in access to surgical care
Progress towards universal access to safe, affordable surgical care is dangerously off track as at least 160 million patients are unable to receive surgery each year, a recent study reveals. “Surgical Health Policy 2025–2035: Strengthening Essential Services for Tomorrow’s Needs” was published in The Lancet on July 14 by the University of Birmingham-led NIHR Global Health Research Unit on Global Surgery.
Low- and middle-income countries (LMICs) bear the brunt of the crisis. Only 26% of LMICs are on track to meet a target for everyone to be able to access essential surgery within two hours, and none have achieved the recommended surgical volume of 5,000 procedures per 100,000 people per year.
Beyond access, quality of surgical care remains a key concern, with 3.5 million adults worldwide dying within 30 days of surgery, considerably more than the combined 2 million adult deaths attributable to HIV/AIDS, tuberculosis, and malaria. Overall, 50 million patients worldwide suffer postoperative complications every year, with wound infection being the most frequent complication. Surgery is a key contributor to antimicrobial resistance, with up to 96% of infected wounds in LMICs being linked to antimicrobial resistance.
Senior author Aneel Bhangu, professor of surgery and director of the Surgical Data Institute at the University of Birmingham, commented: “Surgery is not a luxury. It is a lifesaving, cost-effective intervention that underpins resilient health systems. Without urgent investment, millions will continue to suffer and die from treatable conditions.”
Co-author Rifat Atun, professor of global health systems, vice dean for non-degree education and innovation, and director of the Harvard Health Systems Innovation Lab, added, “Surgery is an integral and indispensable part of universal healthcare coverage. Surgical Health Policy 2025-2035 provides an important roadmap for scaling surgical innovation for those who do not have access to surgery and thus suffer needlessly.”
A global coalition of health experts is calling for urgent access to resolve this crisis. Researchers have made several key recommendations, including:
- Reframing surgery as a foundational component of well-integrated health systems, rather than a siloed intervention. Investing in surgery can boost patient care across numerous diseases by increasing access to diagnostics, intensive care, and critical drugs.
- Unlocking a “surgical prosperity dividend” by increasing access to essential surgery. For example, scaling up breast, stomach, colon, and rectal cancer surgery in LMICs could enable 884,000 people to return to work and boost the global economy by over $80 billion each year.
- Developing innovative funding models for surgery. Half of patients currently undergoing cancer surgery in LMICs make out-of-pocket payments which can result in catastrophic expenditure and poverty.
Read the full article here: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(25)00985-7/abstract
Last Updated
This dietary pattern could save lives and the planet

Some 40,000 early deaths could be prevented each day across the world if more people adopted a healthier, planet-friendly diet, according to a new landmark report. The findings from the 2025 EAT-Lancet Commission on healthy, sustainable, and just food systems, released Oct. 2, also suggest that widespread global adoption of a diet emphasizing minimally processed plant foods could result in greenhouse gas emissions from agriculture being cut by more than half.
The report builds on the 2019 EAT-Lancet report, which first dubbed this dietary pattern the Planetary Health Diet. Commission co-chairman Walter Willett, professor of epidemiology and nutrition at Harvard T.H. Chan School of Public Health, was quoted in multiple news stories about the new report.
“The Planetary Health Diet is not a one-size-fits-all approach,” he said in an Oct. 2 ABC News article. “It allows for cultural diversity and individual preferences, providing flexibility within clear guidelines to achieve optimal health and sustainability outcomes worldwide.”
What variations of the Planetary Health Diet have in common are a focus on fruits, vegetables, nuts, legumes and whole grains, with moderate amounts of meat and dairy and very little added sugar, saturated fat, and salt, Willett said in an Oct. 2 CNN article. He suggested limiting dairy to once a day, red meat to once a week, and eggs, poultry, and fish to about twice a week.
Members of the Commission—who include experts in nutrition, climate, economics, health, and agriculture from more than 35 countries—found even greater population health benefits to widespread adoption of the Planetary Health Diet than in the 2019 report. They increased their estimate of annual lives saved from 11.6 million to 15 million and also noted associations with reductions in cancer and neurodegenerative diseases, and other improved chronic disease outcomes.
Read the report: The EAT–Lancet Commission on healthy, sustainable, and just food systems
Read ABC News article: Landmark study recommends ‘Planetary Health Diet’ for saving lives and the planet
Read the CNN article: Aplanet-first diet can feed the world by 2050 while improving the environment, new scientific analysis finds
Read a Guardian article: ‘Planetary health diet’ could save 40,000 deaths a day, landmark report finds
Learn more
Planetary Health Diet associated with lower risk of premature death, lower environmental impact (Harvard Chan School news)
Last Updated
Featured in this article
Bridging the partisan divide on climate change

When it comes to climate change solutions, Gina McCarthy and Bob Inglis agree that, in spite of the Trump administration pulling back on regulations to curb the use of fossil fuels, there are things to be hopeful about.
Inglis, former Republican U.S. Congressman from South Carolina, and McCarthy, former administrator of the U.S. Environmental Protection Agency during the Obama administration, spoke at an Oct. 6 panel hosted by The Studio at Harvard T.H. Chan School of Public Health focused on finding bipartisan solutions to climate change during turbulent times. The event was moderated by Gaurab Basu, assistant professor in the Department of Environmental Health and a faculty member at the Center for Climate, Health, and the Global Environmental (Harvard Chan C-CHANGE).
Inglis said he finds hope in the fact that businesses are pursuing sustainable options even without being forced to by the federal government. For instance, he noted that Ford is stepping up production of electric cars to better compete in Europe, where EV sales are on the rise. Referring to Trump administration priorities, he said, “Eventually shaky ideologies are overcome by the facts—especially economic facts.”
McCarthy—who also previously served as C-CHANGE director—said that “this has been the most challenging time I have ever had to live through. It’s very difficult to see science being denigrated.” But she has found venues where she tries to make change, such as America Is All In, a coalition of leaders across the U.S. working to support climate action. “When the federal government isn’t working on our behalf, there are other venues to actually make progress,” she said.
Basu asked Inglis and McCarthy why they care so much about climate change. McCarthy recalled being aware from a young age “that we had huge challenges, both health and environmental. When I grew up, everything was dirty. There was pollution spewing everywhere, we had water contamination everywhere.” She became further engaged in climate issues while serving as the health agent in Canton, Mass. She later worked in various environmental roles in Massachusetts and Connecticut, eventually moving on to federal roles, including White House national climate adviser under President Joe Biden.
As for Inglis, he admitted that he didn’t always care about climate change. During his first stint in Congress from 1993-99, he thought it was “nonsense.” But in 2004, when he had the opportunity to run for the same seat again, he was pushed to think differently about the issue when his son—who was turning 18—said he’d vote for him only if he “cleaned up his act on the environment.” The rest of Inglis’s family agreed.
Later, back in Congress, Inglis took trips to Antarctica and Australia’s Great Barrier Reef, where he witnessed climate-related damage firsthand. In 2009, he introduced a bill that would’ve instituted a carbon tax while reducing Social Security taxes. Although the bill failed, Inglis said that he still thinks such a tax would make sense. “If you don’t want to regulate something, you tax it,” he said.
To engage conservative voters on the issue of climate change, Inglis suggested using messaging aimed at right-of-center voters, focused on issues such as how climate action can boost the economy and create jobs. He thinks the climate conversation has mostly been in the “language of the left”—focused on protecting the community as a whole and on fairness—which may not resonate as much with voters on the right.
McCarthy said it’s important to talk about the science of climate change, “but we have to bring it to life. We have to ground [the science] by talking about what it means for everyday people’s human needs.”