Climate-Smart Public Health: A blueprint for resilient health systems

Until now, systems that collect public health information haven’t been connected to data about the climate and environment, making it difficult to anticipate how climate change impacts people’s health. When these different types of data are brought into one platform, researchers and climate and health practitioners can better understand how environmental changes lead to infectious diseases, chronic health conditions, and issues related to nutrition and mental health, which can improve development of early warning systems and public health measures that are more responsive to climate change.
In a new article in The Lancet Planetary Health, our core faculty member Christopher Golden introduces the concept of “Climate-Smart Public Health” (CSPH), a data-driven framework designed to monitor, assess, and adapt to climate-related health impacts, especially in under-resourced regions most vulnerable to climate impacts. The article offers a concrete, scalable blueprint that governments can adopt or adapt, creating operational solutions for climate-resilient health systems.
How Climate-Smart Public Health Can Make Public Health Systems More Effective
CSPH incorporates surveillance, risk assessment, early warning systems, and resilient healthcare infrastructure and introduces innovations that empower policymakers and healthcare professionals with data-driven decision-making. It does this by:
- Integrating inputs from local communities, health practitioners, and implementation organizations to develop a nuanced understanding of health vulnerabilities.
- Using an adaptive approach that allows the system to evolve based on feedback and real-world experience.
- Building an understanding of vulnerabilities from the bottom up, ensuring solutions are locally relevant and inclusive.
- Emphasizing flexibility to address the impacts of changing and evolving climate hazards.
Additionally, CSPH uses data science and AI to address a wide range of health issues, including infectious diseases, non-communicable diseases, nutrition, and mental health.
Climate-Smart Public Health in Action
The article explores how Golden’s research team put CSPH into action in Madagascar, a critical location to launch CSPH due to high rates of poverty, malnutrition, and maternal mortality, alongside frequent cyclones, floods, heatwaves, and droughts. Because of its vulnerability to climate impacts and ongoing preparedness efforts, Madagascar is an ideal setting to develop CSPH interventions that can serve as models for other vulnerable regions globally.
Golden’s research team brought CSPH to life through two specific projects: monitoring droughts to assess the risk of crop failures and associated malnutrition, and detecting harmful algal blooms and monitoring the population for marine food poisoning. The article describes how the team successfully implemented CSPH by:
- Merging health data from thousands of health clinics with climate and environmental data like remote sensing of temperature, rainfall, and crop status.
- Using AI and satellite imaging to monitor and predict drought and harmful algal blooms.
- Partnering with Madagascar’s Ministry of Public Health and other ministries and NGOs to build interoperable databases and ensure findings informed public health planning and early warning systems.
- Creating high-resolution, time-specific risk maps and early warning alerts that guided real-world interventions, such as targeting food aid and health resources to impacted communities.
The four pillars of Climate-Smart Public Health
The four pillars of Climate-Smart Public Health—surveillance and monitoring, risk assessment, early warning and response, and resilient health infrastructure—offer a scalable, data-driven framework, and the authors demonstrate how the strategies used in Madagascar can be tailored and implemented in diverse settings worldwide.
Surveillance and Monitoring
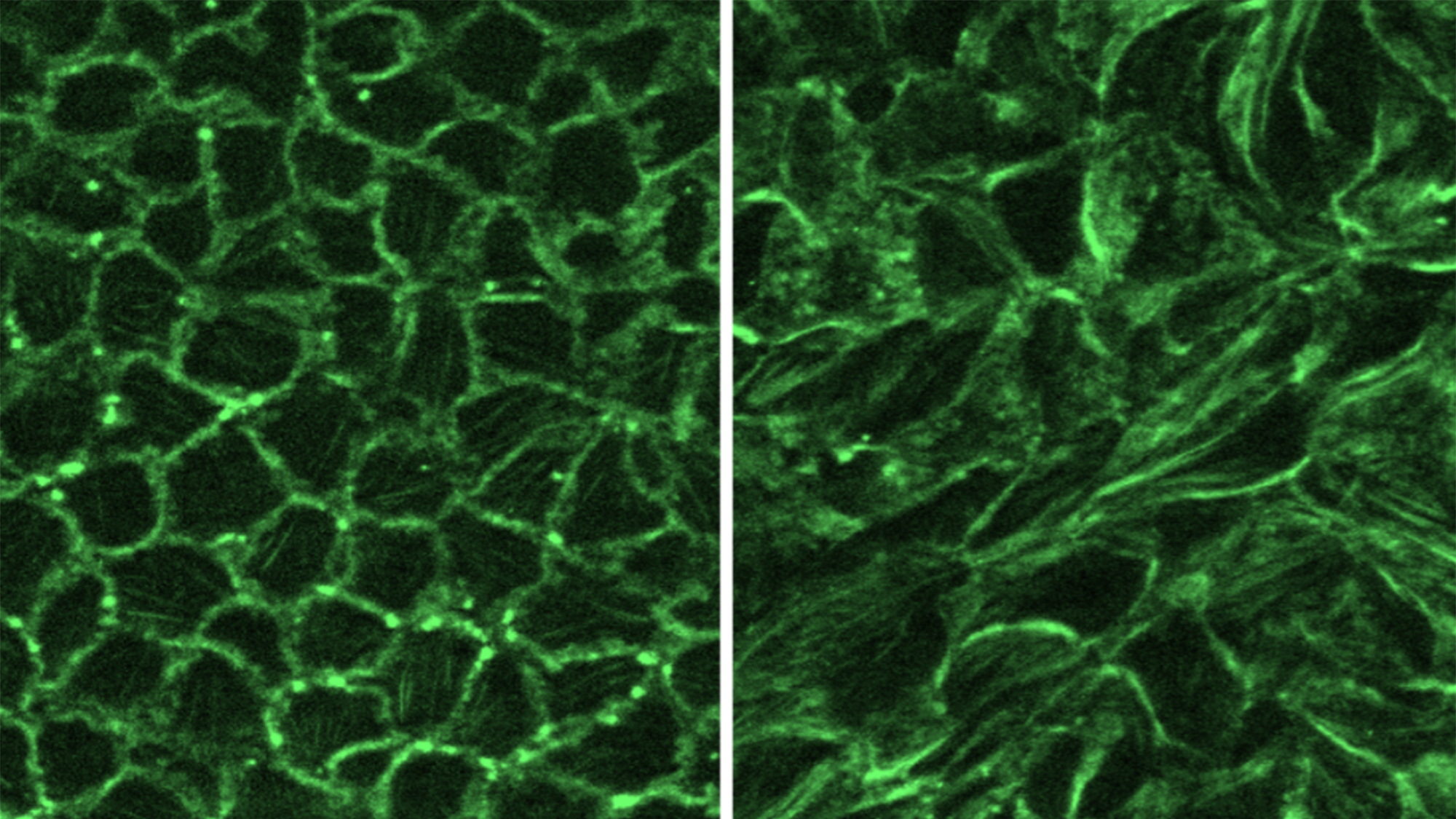
CSPH begins with integrated surveillance of climate, environmental, and health data to track how climate factors influence health outcomes. In Madagascar, researchers combined clinic-based health data with climate datasets (e.g., temperature, rainfall) and remote sensing to map disease trends and environmental exposures over space and time. By building an interoperable data platform and leveraging ground-based sensors for local accuracy, the project overcame infrastructure limitations common in resource-limited settings.
Takeaway: To implement surveillance and monitoring successfully, prioritize linking routine health data with openly accessible climate information, and use low-cost sensors to fill data gaps for real-time, location-specific monitoring.
Risk Assessment
CSPH calls for systematic evaluation of the health risks posed by climate-related threats like droughts, floods, and extreme heat. The team in Madagascar linked climate stressors (e.g., drought) to agricultural production declines and malnutrition, using AI to analyze spatial connections between weather and health records. Vulnerability mapping identified populations most at-risk.
Takeaway: Use health, demographic, and climate data to model exposure-response relationships, identify at-risk groups, and guide resource priorities. Build risk maps to inform targeted interventions. Even with limited data, combining local knowledge and available remote-sensing technologies can reveal critical risk patterns.
Climate-Smart Early Warning and Response Systems
Effective CSPH includes data-driven early warning systems to predict and address imminent health threats from climate hazards. In Madagascar, AI and remote sensing predicted droughts and harmful algal blooms, enabling local agencies to issue targeted food and health alerts. Collaboration with government ministries ensured that advance warnings could prompt timely local responses.
Takeaway: Start by integrating weather forecasts, remote sensing, and existing health surveillance to develop early alerts for officials and communities. Partner with local agencies to determine the most useful warning timescales and ensure warnings reach those who can act. Digital and radio alerts work well in low-resource environments.
Climate-Smart Health Infrastructure and Provider Capacity
CSPH strengthens healthcare facilities and trains providers to withstand and adapt to climate stressors. Madagascar will need climate-resilient clinic design (e.g., flood-resistant materials, solar power) and updated health worker training to recognize climate-sensitive diseases and adapt during extreme weather.
Takeaway: Assess healthcare facility locations and vulnerability to climate hazards, and plan upgrades (energy, water, sanitation) for resilience. Invest in ongoing training so providers can identify and treat emerging climate-related health conditions. Collaborate with local authorities to mainstream these standards and ensure system-wide buy-in. Adapt training and infrastructure upgrades based on local climate risks and community needs.
Applications for International Health Care Policy
To protect people from the increasing health threats caused by climate change, countries need stronger, more adaptable public health systems. Extreme weather, food insecurity, and the spread of disease are becoming more common, making it vital for health services to be ready and resilient. Many nations, including Madagascar, have committed to building climate-resilient healthcare systems, supported by global organizations such as the World Health Organization (WHO) and the Alliance for Transformative Action on Climate Change and Health (ATACH). These efforts depend on cooperation between government agencies, scientists, and communities to set shared goals and ensure effective leadership, resources, and training.
A key part of this strategy is the use of reliable data about health, climate, and the environment. Tools such as CSPH help combine these different data sources to provide early warnings and guide action where it’s needed most. By developing adaptable digital platforms and sharing lessons learned in Madagascar, this approach can be used by countries everywhere to target health risks from climate change and build more resilient futures for all.