Center for Work, Health, and Well-being
The Center for Work, Health, and Well-being is a multidisciplinary center advancing worker safety, health, and well-being through research and dissemination of evidence-based practices, programs, and policies.
Kresge Building, 7th floor
677 Huntington Avenue
Boston, MA 02115
Research
The Center collects and analyzes data, conducts intervention research and implementation studies, and develops evidence-based evaluation tools, models and frameworks to help both researchers and practitioners understand the connections between work and working conditions; worker safety, health and well-being; and business outcomes. Our research engages key stakeholders in its development, implementation, evaluation and the translation of research findings into practice through our outreach efforts and dissemination of resources.
Findings from the Center’s research provide the evidence needed to develop and implement policies, programs and practices that improve working conditions in support of worker health, safety, and well-being across many industries.
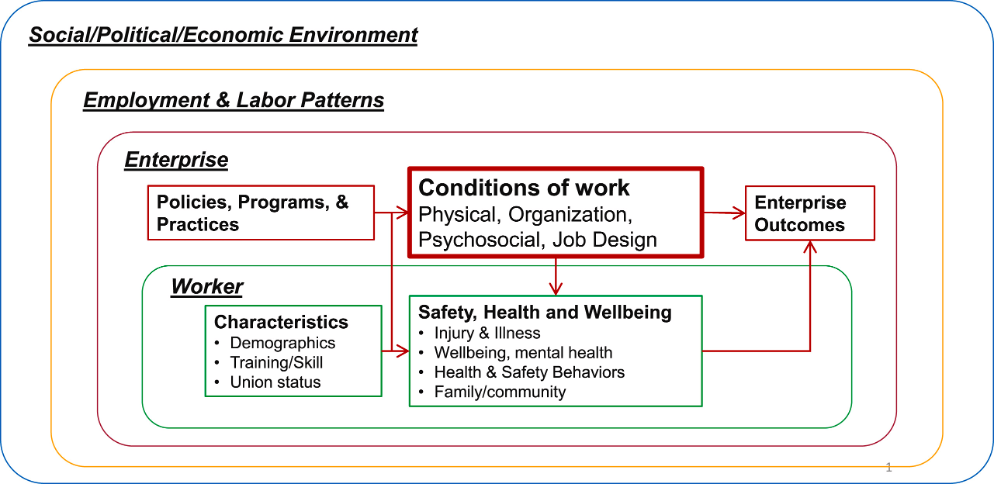
Based on more than 20 years of research in multiple industries, the Center’s conceptual model identifies the many pathways that concurrently influence worker health, safety, and well-being. Central to the model is the focus on conditions of work, which contribute to workers’ safety, health and well-being as well as to organizational outcomes such as increased productivity and reduced turnover, absences, and healthcare costs. This framework guides the Center’s research and enables us to design and test interventions meaningful to both workers and employers. It also allows for the development and implementation of policies and practices tailored to an organization’s specific conditions of work, including the physical work environment and the organization of work.
The Center’s conceptual model for protecting and promoting worker health, safety, and well-being:
Boston Hospital Workers Health Study (2007-2026)

Description: The Boston Hospital Workers Health Study seeks to determine how workplace exposures, structures, and policies in hospitals contribute to worker health, safety, and well-being. The goal of this study is to improve the health of the hospital workforce and reduce within-workforce disparities by identifying root causes in the conditions of work. The Center has a long-standing collaboration with two large hospitals in Boston, Massachusetts. Using the hospitals’ longitudinal database of employee records, the Center’s research seeks to identify ways in which working conditions, including workplace exposures and policies, impact worker health, safety, and well-being, especially for low-wage workers. Researchers explore how policies aimed at improving working conditions have the potential to narrow or widen occupational, wage and other gaps in health within the hospital workforce. This work broadens the scope of occupational health research and practice in hospitals, as it demonstrates the benefits of examining working conditions and policies to identify opportunities to better support the safety, health and well-being of the hospital workforce.
Key Findings: The Boston Hospital Workers Health Study has explored multiple topics since it began in 2007. The many evidence-based findings from this study have informed policy and practices at the collaborating hospitals; those policies and practices are then able to be studied due to the longitudinal data that has been collected (a cycle of research-to-practice-to-research). Some of the Center’s findings include that increased frequency of specific types of experiences (particularly being unfairly humiliated in front of others and being watched more closely than other workers) was associated with progressively greater odds of injury at work. Another analysis demonstrated that active and high strained healthcare workers were associated with higher odds of experiencing burnout, as were workers who reported perceived low workplace flexibility. Another analysis showed that workers experiencing incivility or bullying in the workplace had greater odds of mental health claims, suggesting that workplace incivility and bullying may carry monetary costs to employers, which could be controlled through work environment modification.
Additional findings from other analyses of the Boston Hospital Workers Health Study data are summarized below.
Principal Investigators: Erika Sabbath (2016-2025) and Glorian Sorensen (2007-2016)
Funder: National Institute for Occupational Safety and Health
Vicarious Occupational Trauma Exposure Index (2022-2025)
Description: Many professionals who work with people who have trauma histories experience vicarious trauma. Vicarious trauma is “second hand” trauma that is passed on to workers when they interact with individuals who experienced trauma “firsthand” or encounter information about the trauma. A worker may not directly experience the trauma, but because they work with people or communities that have, the worker may experience these traumas indirectly. Vicarious trauma can negatively affect the mental and physical health of professionals through psychological and physiological stress-response pathways. The Vicarious Occupational Trauma Exposure (VOTE) Index is a tool designed to identify parts of a worker’s job that expose them to vicarious trauma, how often they are exposed to vicarious trauma, and how strong the vicarious trauma exposure is.
Key Findings: In a study of 775 hospital workers, survey data were linked to health insurance expenditures to identify stress-related conditions known as disorders of gut-brain interaction (DGBIs) occurrence within a one-year follow-up. Vicarious Trauma (VT) symptoms and conditional odds of developing DGBI were assessed with multilevel logistic regression. Conditional odds of DGBI increased 4% for every one-point increase in VT symptom score. Workers with high versus low VT symptoms had significantly higher odds of developing DGBIs, indicating that VT may adversely impact workers’ physical health.
Principal Investigator: Elisabeth Stelson
Funders: National Institute for Occupational Safety and Health, National Institutes of Health, Harvard Chan School Lee Kum Sheung Center for Health and Happiness
Workplace Violence among Hospital Patient Care Employees (2023-2024)
Description: The Characterizing Experiences of Workplace Violence among Hospital Patient Care Employees study used data from the Boston Hospital Workers Health Study for a mixed-methods pilot exploring causes of workplace violence among nurses and patient-care associates. The project aimed to understand what policies can better protect these workers before, during, and after a violent incident. Within an established occupational cohort study, the researchers analyzed multiple data sources (survey data, injury reports, and semi-structured interviews) and integrated them with relevant social theory to understand violence as a continuum.
Principal Investigators: Erika Sabbath and Ricardo Diego Suárez Rojas
Funder: National Institute for Occupational Safety and Health
Positive Working Conditions for Patient Care Workers in Hospital Settings (2018-2019)
Description: The goal of the Investigating facilitators and barriers to the implementation of policies, programs, and practices supportive of positive working conditions for patient care workers in hospital settings study was to identify facilitators of and barriers to the implementation of hospital policies related to organizational and psychosocial working conditions of Patient Care Workers in acute-care settings. This study used worker survey and medical claims data from a sample of patient-care workers from the Boston Hospital Workers Health Study to assess the relationship of psychosocial (job demands, decision latitude, supervisor support, coworker support) and organizational (job flexibility, people-oriented culture) working conditions with self-reported mental health and mental health expenditures.
Key Findings: People-oriented culture and coworker support were negatively correlated with psychological distress and were predictive of lower expenditures in mental health services. Job demands were positively correlated with psychological distress.
Principal Investigator: Maria Lopez Gómez
Funder: National Institute for Occupational Safety and Health
Return-to-Work Following Work-Related Injury in Patient Care Workers (2018-2019)
Description: Hospital patient care workers are at increased risk of injury as a result of hazards in their work environment, psychosocial work stressors, workplace culture, the organization of their work, and their interactions with patients. Because of this, healthcare workers have some of the highest rates of injuries, workers’ compensation claims, and prolonged periods off work. This study explored the conditions of work and contextual mechanisms that influence return-to-work following work-related injury in a cohort of patient care workers, exploring how organizational policies and practices, conditions of work, individual worker factors, and other potential mechanisms influenced the return-to-work process and the experiences of workers and nurse managers.
Key Findings: Different hospital units had different working conditions and demands which influenced both the nature and type of work-related injuries as well as the return-to-work process.Psychosocial working conditions such as supervisor and coworker support were considered the most important for workers staying at work (rather than taking a leave of absence after their injury); this also impacted whether workers felt comfortable reporting injuries to their nurse director.
Principal Investigator: Susan Peters
Funder: National Institute for Occupational Safety and Health
For more than a decade, the Center has been studying the concept of thriving from work, building on many years of research on worker well-being. Grounded in our research, well-being theory, and current evidence, Dr. Susan Peters has led researchers in the development, validation and implementation of a model for Thriving from Work. Thriving from Work is a composite integrated well-being construct that encapsulates how the experience of work and working conditions has a positive influence on the well-being of workers, not only at work but also in their lives outside of work. Thriving from Work is defined as the state of positive mental, physical, and social functioning in which workers’ experiences of their work and working conditions enable them to thrive in their overall lives, contributing to their ability to achieve their full potential in their work, home, and community.
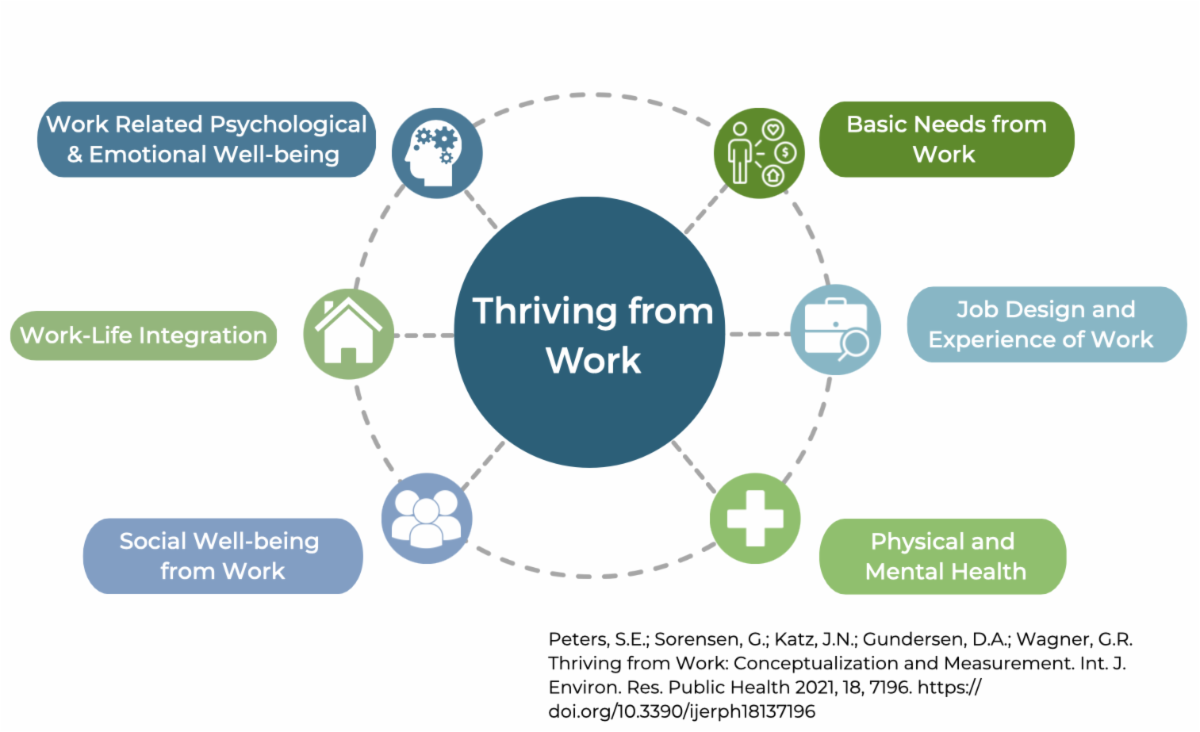
Based on this conceptualization of Thriving from Work, Center researchers developed a questionnaire to measure thriving from work in addition to being a ‘diagnostic tool’ to identify areas within an organization that would benefit from well-being policies, programs and practices. The Thriving from Work Questionnaire (TfWQ) also helps organizations identify “what” dimension of well-being needs improvement to guide specific intervention design. This questionnaire has been translated into several languages and has been validated in different geographic and occupational contexts.
Research is continuing and is currently focused on several topic areas, each of which is focused on thriving workers and thriving workplaces.
For further inquires please contact Susan Peters at sepeters@hsph.harvard.edu
Thriving Workers, Thriving Workplaces Study (2022-2026)
Description: The Thriving Workers, Thriving Workplaces Study seeks to identify relationships between workers’ thriving from work and working conditions, workplace policies, and workplace practices. Thriving from work is defined as the state of positive mental, physical, and social functioning in which workers’ experiences of their work and working conditions enable them to thrive in their overall lives, contributing to their ability to achieve their full potential in their work, home, and community. To examine thriving from work across multiple work settings, this study uses cross-sectional data from hospital workers and warehouse workers to identity how working conditions and worker characteristics are associated with workers’ thriving.
Based on formative research in multiple industries and occupational roles, the Thriving from Work Questionnaires enable measurement of the extent to which workers are thriving from their day-to-day work, and identify priority areas for intervention. This research examines policies, programs, and practices that influence thriving from work, as well as making the business case for investing in worker well-being by studying the relationship between thriving from work and key organizational outcomes such as turnover, performance, and occupational injury.
Principal Investigators: Susan Peters and Gregory Wagner
Funder: National Institute for Occupational Safety and Health, Harvard Chan School Lee Kum Sheung Center for Health and Happiness
Thriving from Work: Assessment and Impact of Older Worker Preferences (2024-2025)
Description: Despite the known benefits of work and the disparities that exist in access for older workers, little is known about what workplaces can do to retain and support older workers. This project builds on existing survey tools to pilot a valid measurement approach of older worker preferences as predictors of thriving from work and retention. The study collected survey data from 1,000 working adults over age 50 to understand their work preferences, working conditions and work arrangements and the relationship with thriving from work to support the validation of the Thriving from Work Questionnaire with this demographic. These were compared with a sample of younger workers.
Principal Investigators: Susan Peters, Cal Halvorsen, Maren Voss
Funder: National Institute for Occupational Safety and Health

Description: The Fulfillment Center Intervention Study evaluated a participatory, prevention-oriented approach that aims to change conditions of work to reduce the risk of poor mental health, improve workers’ well-being, and reduce levels of unreported injuries in warehouse fulfillment centers. These workers have physically taxing and high-strain jobs, often with high demands and limited control over working conditions; this may negatively impact mental and physical health, including injury-related disability. The study evaluated the implementation of a workplace intervention which introduced “Health and Well-being Committees” that solicit and prioritize workers’ concerns regarding working conditions, and implement action plans to address them, creating a new channel for worker input into the conditions of work. The research tested the hypothesis that the intervention modifies working conditions to improve mental health and psychological well-being, reduce injuries, and encourage injury reporting. This project also explored key contextual factors that support effective implementation and sustained engagement.
Key Findings: The research team found that after six months, employees in the buildings with Health and Well-being Committees were 33% less likely to report moderate or severe psychological distress than employees in the other buildings. The researchers also found a striking reduction in employee turnover, which was welcome news for the employer, since high turnover results in higher training costs and lower productivity. Employees in the buildings with a Health and Well-being Committee had a 20% lower probability of exit compared to the previous year’s exit rates. The researchers observed that employees benefited from having a voice and a chance to share their concerns — being respected, heard, and valued as a member of the organization in a very regimented, technologically monitored setting.
Principal Investigators: Erin Kelly and Lisa Berkman
Funder: National Institute for Occupational Safety and Health
Description: The Older Workers’ Health and Well-being Study examines how access to workplace benefits and policies are associated with older workers’ physical and mental health as well as enjoyment in going to work. These may include, for example, employer-provided health insurance, retirement savings programs, and the ability to reduce hours. This project explores working conditions as critical determinants of health and well-being, providing opportunities to study differences in these relationships. Based on analysis of six waves of the Health and Retirement Study of Americans, this study spotlights the importance of supporting older workers, a growing part of the workforce, and was developed to address concerns about the health, safety, and well-being of the older workforce. It is projected that by 2050, 24% of the U.S. labor force will be made up of workers aged 55 years and older, up from 13% in 2000.
Key Findings: This analysis showed that roughly two in five workers aged 50-64 did not have access to employer-provided health insurance nor retirement savings programs during the study period. Moreso, this analysis shows that about seven in ten older workers did not report the ability to reduce their working hours. While some differences were noted by gender and race, the biggest differences were by ethnicity, with non-Hispanic older workers reporting access rates that were 20 and 30 percentage points higher than their Hispanic counterparts on access to employer-provided health insurance and retirement savings programs, respectively.
Principal Investigators: Cal Halvorsen and Erika Sabbath
Funders: AARP Thought Leadership and the National Institute for Occupational Safety and Health
Description: Non-uniformed responders such as construction, electrical, and transportation workers, worked alongside uniformed responders during the World Trade Center (WTC) rescue, recovery and clean up. Like their uniformed counterparts, non-uniformed responders were exposed to traumatic destruction and loss of life as well physical, environmental, and psychological hazards. The World Trade Center Non-Traditional Responders’ Employment and Mental Health Study sought to understand how responders’ experiences onsite impacted their employment and mental health over the 20+ years since September 11, 2001. This study also explored how various onsite supports, social relationships, and work experiences post 9/11 impacted their mental health and employment trajectories. WTC non-uniformed responders have experienced higher rates of poor mental health than uniformed responders, yet there has been little study as to why this has been observed. Similarly, there has been little research focused on how WTC non-uniformed responders’ experiences impacted their employment trajectories after 9/11. This study utilized longitudinal data from the WTC General Responder Cohort of over 45,000 responders, as well as collecting new data using interviews and surveys.
Principal Investigator: Susan Peters
Funder: National Institute for Occupational Safety and Health

Description: In the wake of the US Supreme Court’s 2022 Dobbs v Jackson Women’s Health Organization decision, which overturned federal protections on abortion, obstetrician-gynecologists (OB-GYNs) face policy-related threats to their personal and professional well-being. The Study of OB-GYNs in Post-Roe America (SOPRA) investigates the relationships between state abortion policy environments, OB-GYNs’ work experiences and stressors, and their health and well-being. It also identifies organizational-level policies and practices that may buffer negative effects of policy-related stressors on OB-GYNs. By generating rigorous scientific evidence and actionable recommendations to help healthcare organizations support OB-GYNs, SOPRA aims to protect and promote the health and well-being of this essential workforce. For more information, please visit the SOPRA study website here.
Key Findings: During interviews with 54 OB-GYNs practicing under abortion bans in 13 states, participants described a range of perceived impacts, including distress at having to delay essential patient care, fears of legal ramifications, mental health effects, and planned or actual attrition. These findings have implications for workforce sustainability, physician health, and patient outcomes. In the context of public policies that restrict physicians’ clinical autonomy, organization-level supports for physicians are essential to maintain workforce sustainability, clinician health and well-being, and availability of timely and accessible health care throughout the US.
Principal Investigators: Erika Sabbath and Mara Buchbinder
Funders: Greenwall Foundation (2023-2024), National Institute for Occupational Safety and Health (2024-2027)

Multiple intervention studies have been conducted focusing on general contractors and subcontractors in commercial construction, an industry with highly dynamic work environments and significant physical hazards. Workers are more prone to injuries, including musculoskeletal disorders, and high-risk health behaviors, such as tobacco use. Construction workers also have some of the highest rates of poor mental health, substance use, and opioid overdose, compared to the overall U.S. working population.
All the Right Moves: Intervention to Improve Worker Safety and Health (2016-2017)
Description: This study evaluated the efficacy of “All the Right Moves”, a program designed to target the conditions of work and workers’ health behaviors through an ergonomics program combined with a worksite-based health promotion Health Week intervention, at the general contractor level. This was tested using a matched pair, cluster randomized controlled trial. The program was evaluated by collecting surveys before the intervention was implemented and at one and six months after the intervention was completed. These were supplemented with focus groups and manager interviews as well as intervention process evaluation data.
Key Findings: “All the Right Moves” demonstrated that an integrated Total Worker Health® approach integrating health promotion (“Health Week”) with injury prevention (ergonomics program) can reduce injuries and spark healthier eating and recreational physical activity behaviors, even in fast-paced construction settings. At one-month following the ergonomics program, researchers observed a significant improvement in ergonomic practices, and a reduction in incidences of pain and injury in the intervention group. At six months, the researchers observed differences in favor of the intervention group for a reduction in physically demanding work, increased recreational physical activity and higher consumption of fruits and vegetables. Process evaluation of the intervention revealed several barriers to intervention implementation fidelity and uptake, including a multiemployer worksite, the itinerant nature of workers, competing production pressures, management support, and inclement weather. The research suggests that to sustain and scale these gains, owners and general contractors need to address structural barriers in multi-employer worksites and commit to longer-term, upstream solutions. These findings need to be considered in designing, implementing, and sustaining Total Worker Health interventions on construction worksites.
Principal Investigator: Jack Dennerlein
Funder: National Institute for Occupational Safety and Health
All the Right Moves for Subcontractors: Intervention to Improve Worker Safety and Health (2017-2020)
Description: The goal of this project was to improve the overall well-being of construction workers employed by subcontracting companies through a participatory intervention. The intervention was designed to improve worker voice as a mechanism for identifying and remediating stressful and problematic working conditions and practices on site to better support worker safety, health, and well-being. The first step was to develop and pilot the intervention. The researchers then examined the effectiveness of the intervention using a stepped-wedge cluster randomized controlled trial. Survey, interview, and process evaluation data was collected from all companies that participated.
Key Findings: The researchers noted challenges faced by construction subcontractors that they then considered in the intervention design. They developed a communication infrastructure company-based, continual improvement, participatory intervention design, consisting of a needs assessment and report, committee-led prioritization, action planning and implementation, and worker communication/feedback cycle. The study contributed to the final intervention design with modifications made with respect to timing, implementation support, capacity building, adaptability and sustainability.
Principal Investigator: Jack Dennerlein
Funder: National Institute of Occupational Safety and Health
Resources: The Center developed a series of Toolbox Talks as part of the All the Right Moves (ARM)and All the Right Moves for Subs (ARM for Subs) Programs with construction workers. These Toolbox Talks fall into three categories: Respiratory Health, Safety Climate, and Work Life – three areas our research has shown are of significant importance in the construction industry. Programs to improve construction worker health, safety, and productivity often incorporate Toolbox Talks on relevant topics. These short facilitated interactive discussions provide opportunities for learning and also for workers to share their experiences and suggestions. These are available on our resources page.
B-SAFE: Safety communication and recognition program for commercial construction worksites (2009-2014)
Description: B‐SAFE, a safety communication and recognition program, facilitates communication between workers and management of all levels on hazard recognition and controls, and provides the site with a free lunch and raffle when a high level of safety is achieved.
The program was piloted for two months on a commercial construction worksite and then redesigned using qualitative interview and focus group data from management and workers. The researchers then ran the redesigned program for six months on the same worksite. Foremen received detailed weekly feedback from safety inspections, and posters displayed worksite and subcontractor safety scores. In the final program design, the whole site, not individual subcontractors, was the unit of analysis and recognition.
Key Findings: The B‐SAFE program led to many positive changes, including an improvement in safety climate, awareness, teambuilding, and communication. This program received high levels of acceptance from workers, who noted increased levels of site unity and team-building. This pilot program showed that construction workers value solidarity with others on site, demonstrating the importance of health and safety programs that engage all workers through a reliable and consistent communication infrastructure.
Principal Investigators: Jack Dennerlein, Emily Sparer-Fine
Funder: National Institute for Occupational Safety and Health
Opioid Use in Construction (2019-2020)
Description: Commercial construction workers have the highest opioid-related fatalities of any occupational group in the United States, with the majority of these overdose deaths related to a history of work-related injury.
Using focus groups with construction workers, and interviews with construction managers and leaders, this qualitative study had two aims: (1) to identify and examine the contextual factors influencing the delivery and evaluation of a planned employer-based program, and (2) to develop and test an outcome measure of workplace health climate focusing on pain and pain management, including opioid use and addiction.
Key Findings: The outputs of this research activity included new knowledge about pain and pain management for workers, a new scientific instrument to help evaluate organizational climate surrounding worker pain and pain management, and the groundwork for a new intervention model for opioid addiction prevention within the community.
Principal Investigator: Jack Dennerlein
Funder: Northeastern University
Mental Health in Construction (2016-2017)
Description: This study determined what workers think about and what they understand about their mental health and well-being within the context of the work environment, including factors that contribute to poor mental health and those that support and promote mental health and well-being. The study examined pathways within the Center’s Conceptual Model by testing associations between work-related factors and psychological distress among commercial construction workers. The study also sought to understand the relationship between mental health stigma and wellbeing in a sample of commercial construction workers
Key Findings: Stigma was significantly associated with psychological distress and impaired sleep, but not with substance abuse. Workers discussed the prominence of stigma on worksites and how the masculine culture of the industry and job insecurity contributed to stigma. This stigma poses a barrier to addressing mental health among workers.
Principal Investigator: Jack Dennerlein
Funder: National Institute for Occupational Safety and Health
Description: The Low-Wage Workers in Nursing Homes study sought to establish the degree to which the nursing home industry’s existing programs, policies, and practices align with the Total Worker Health® approach, specifically as it relates to a reduction in occupational injuries of low-wage workers in nursing homes and improvements in patient outcomes. The U.S. nursing home industry workers are at high risk for chronic disease and occupational injury, and 70% earn low wages. This study utilized the Center’s Workplace Integrated Safety and Health (WISH) Assessment to evaluate how well existing programs, policies, and practices in approximately 500 nursing homes address the safety, health, and well-being of low-wage workers. The project also examined whether ownership and features of occupational health programs are associated with WISH Assessment scores.
Key Findings: In their survey of more than 500 nursing homes in three US states, researchers found a high degree of nursing homes that reported implementing Total Worker Health approaches as measured by the WISH Assessment. They did not find associations between for-profit vs. not-for-profit or corporate vs. non-corporate, and WISH domain scores. Simply relying on ownership status is not sufficient for researchers and policy makers seeking to identify nursing homes that may benefit from the additional implementation of Total Worker Health concepts.
Principal Investigator: Jessica Williams
Funder: National Institute for Occupational Safety and Health
Description: The Center partnered with a large food service company to develop and test policies, programs, and practices to improve the health, safety, and well-being of food service workers in corporate environments. The researchers sought to identify working conditions that can be modified to potentially improve the safety, health, and well-being of workers, developing an integrated intervention targeting safety and ergonomics, work intensity, and job enrichment. The study articulated a systematic approach to designing, implementing and evaluating an organizational intervention. The evaluation identified factors contributing to successful implementation as well as challenges in the process, providing a resource for future interventions and recommendations on evidence-based programs, policies, and practices to improve food service workers’ health, safety, and well-being.
Key Findings: Despite strong support from corporate senior leadership, the research team encountered barriers in the implementation of the planned intervention at the worksite and district levels. These included financial demands that drove work intensity; turnover of site and district managers disrupting continuity in the implementation of the intervention; and staffing constraints that further increased workload and pace of work. Findings underscore the need for ongoing commitment and support from both the parent employer and the clients hosting each food service location.
Principal Investigator: Glorian Sorensen
Funder: National Institute for Occupational Safety and Health
Description: The aims of the Substance Use Treatment Provider Occupational Wellbeing Study included identifying challenging working conditions in residential addiction treatment facilities in Massachusetts from the perspectives of substance use treatment providers and organizational leaders. The research sought to ascertain how these identified challenges as well as supports affect the workers’ psychological and physical safety, health, and well-being at work and at home, and determine how identified challenges and supports affect organizational dynamics and workforce turnover at the treatment facilities, as well as the workers’ intentions to leave the field of addiction services. This study also explored sources of stress and resilience among frontline substance use treatment workers, and their suggestions to improve working conditions and the work environment.
Key Findings: The researchers’ analysis of data from focus groups and interviews revealed how socio-contextual factors originating outside of residential facilities were dominant influences on “downstream” working conditions, worker health, staff turnover, and by extension, client care. Findings indicated that protecting health and well-being of providers—many of whom are in addiction recovery themselves— is integral to improving addiction treatment. From this workforce’s perspective, changes in socio-contextual factors have intensified already challenging working conditions (job demands, pay, advancement), negatively impacting worker health, turnover, and client care. Any interventions to improve treatment outcomes or working conditions in nonprofit addiction facilities must consider larger socio-contextual factors influencing these organizations.
Principal Investigator: Elisabeth Stelson
Funder: National Institute for Occupational Safety and Health, National Institutes of Health
Description: Center researchers partnered with Mutual de Seguridad, a Chilean non-profit workers compensation insurer and healthcare provider, and a Chilean transportation company for a three-year project to develop and pilot a participatory organizational safety and well-being intervention based on our Center’s Implementation Guidelines. The study tested the feasibility of implementing a participatory capacity‑building intervention, aligned with a Total Worker Health® approach and aimed at improving bus driver safety and well‑being. Using a pre‑experimental mixed‑methods design grounded in implementation science, researchers worked with company leadership and workers to co‑design and tailor the intervention. Using grounded theory, the researchers built a visual model mapping the links among relational factors, organizational structures, job demands, and resulting health outcomes. This model guided the design of the subsequent organizational intervention to target the root causes identified. The study identified contextual determinants influencing implementation and described how the organization adapted rapidly in response to external shocks—notably the COVID‑19 pandemic and social/political unrest in Chile. The intervention fostered an agile organizational infrastructure, enabling leaders to respond more effectively to workers’ safety and well‑being needs, even under challenging conditions.
Key Findings: The study identified working conditions that were supportive and those needing improvement for worker safety, health, and well-being. Program elements were integrated through modified policies and practices into existing safety management systems with increased focus on worker engagement. The intervention enabled the organization to create an agile infrastructure, allowing leadership to be more responsive to workers’ safety and well-being needs, even amidst strong external forces undermining worker safety and well-being. The majority of workers were satisfied with the efforts to improve trust and support between drivers and supervisors.
Principal Investigators: Jack Dennerlein and Susan Peters
Funder: Mutual de Seguridad
Description: The Senior Community Service Employment Program (SCSEP) is the sole federal workforce-training program for adults who are 55 and older. Part of the Older Americans Act, SCSEP provides on-the-job training to people with incomes at or below 125% of the federal poverty level. Despite its long history, few program evaluations have been completed. This study builds on a qualitative study by Dr. Cal Halvorsen during the summer of 2020 that revealed how program participation led to increased knowledge and use of food and housing security programs, decreased social isolation and financial stress, and increased confidence, among other findings. This feasibility and acceptability study builds upon these findings and assesses SCSEP’s influence on participant health across multiple domains, including physical (e.g., daily exercise), psychological (e.g., mood), social (e.g., social engagement), financial (e.g., medical costs), and interpersonal (e.g., caregiving needs) health and well-being. This is believed to be the first evaluation of the health and well-being outcomes from SCSEP participation.
Key Findings: Participants reported that the benefits of the program encompassed not only personal finances, but also social engagement and self-confidence. Beyond the program’s primary purpose of on-the-job training, most participants reported that through their participation in SCSEP, they learned about services and supports to help them financially, as well as free or low-cost classes to increase their skills or knowledge. Findings suggest that while participants join SCSEP for help finding a job and the financial support that is a part of the program, they gain additional knowledge about financial, health, and training resources that they then share with others.
Principal Investigator: Cal Halvorsen
Funder: Schiller Institute Grants for Exploratory Collaborative Scholarship program at Boston College

Description: Center researchers partnered with the Boston Fire Department and the Boston Firefighters Union, Local 718 to examine factors in fire stations that may impact firefighter cancer risk. Firefighters are at an increased risk for many types of cancer. Although most studies on this topic focus on exposures encountered while fighting fires, exposures at the fire station are also cause for concern. As a first step, the Center’s team completed a pilot, with the goal of describing air quality within a few fire stations in and around Boston, Massachusetts, and to investigate physical and organizational factors that may influence levels of contaminants in stations. Air sampling was completed at four fire stations in the kitchen, truck bay, and just outside the station, and 7 interviews were conducted with officers at each station to explore health and safety-related organizational policies and practices.
Key Findings: At each station, levels of contaminants were higher in the truck bays than outside the stations or in station kitchens, and air quality levels in truck bays varied considerably throughout the day. Building age, station layout, and ventilation all appeared to impact contaminant levels. The station with the highest exposures in the truck bay had the lowest levels in the kitchen, which was possibly explained by new building materials and effective separation between building zones. The age and layout of the stations appeared to determine the extent to which policies favoring exhaust capture were implemented. Through understanding contaminant variability, researchers are better able to design and test interventions that improve cancer prevention. In addition to journal publications, the Boston Globe, Dana-Farber Cancer Institute, and the Harvard Gazette each featured stories on this collaborative research initiative.
Principal Investigator: Emily Sparer-Fine
Funders: National Institute for Occupational Safety and Health and the National Institutes of Health
Description: Nine focus groups were conducted with 55 leaders, supervisors, and frontline employees at a Veterans Affairs Medical Center to understand how the work environment and conditions of work influence employee safety, health, and well-being; what programs, policies, and practices promote and protect employee safety and health in veterans affairs; and how employee safety, health, and well-being impact the organizational mission.
Key Findings: Employees identified organizational and structural elements of work that impact safety, health, and well-being. Six common themes emerged—stressful working conditions, health hazards, organizational factors, current program knowledge, participation barriers, and program suggestions.
Principal Investigator: Eve Nagler
Funder: Veterans Health Administration