Newly discovered mechanism of mitochondrial dysfunction in obesity may drive insulin resistance and type 2 diabetes
For immediate release: May 28, 2025
Boston, MA—A newly discovered mechanism that leads to liver dysfunction may be a key factor in type 2 diabetes and other metabolic disorders in individuals with obesity, according to a new study led by Harvard T.H. Chan School of Public Health. The dysfunction identified—dysregulated hepatic coenzyme Q metabolism—leads to excessive reactive oxygen species (ROS) produced by mitochondria at a single specific site in an enzyme called complex I. The researchers say the discovery offers a potential path for new, precise treatments for metabolic diseases.
“Our findings provide the first step toward solving a complex problem in the field of metabolic disease research that has stood for three decades,” said corresponding author Gökhan S. Hotamisligil, James Stevens Simmons Professor of Genetics and Metabolism. “Too much ROS has long been linked to obesity and age-related diseases, but precisely why, where, and how excess ROS is produced has remained unknown, limiting progress toward targeted therapeutics. This study helps close those knowledge gaps.”
The study was published May 28 in Nature.
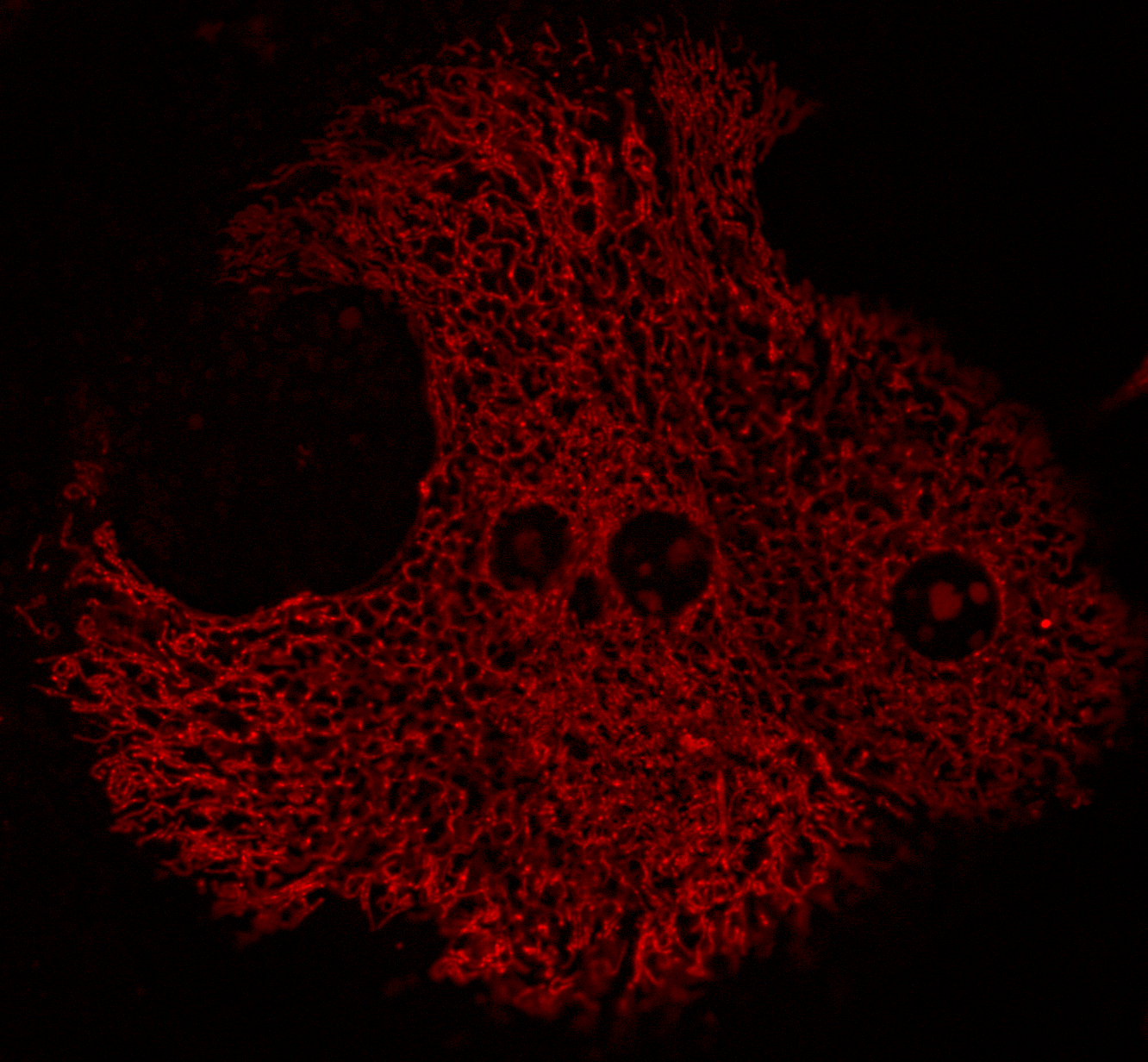
Mitochondria metabolize nutrients and generate the building blocks needed to maintain metabolic homeostasis. During this process, mitochondria also generate ROS—molecules that, in small, controlled amounts, are essential to support normal body functions, but that can be harmful when produced in large quantities. Excess ROS production is a known consequence of obesity, but its relationship to related metabolic disorders, such as type 2 diabetes, has been poorly understood.
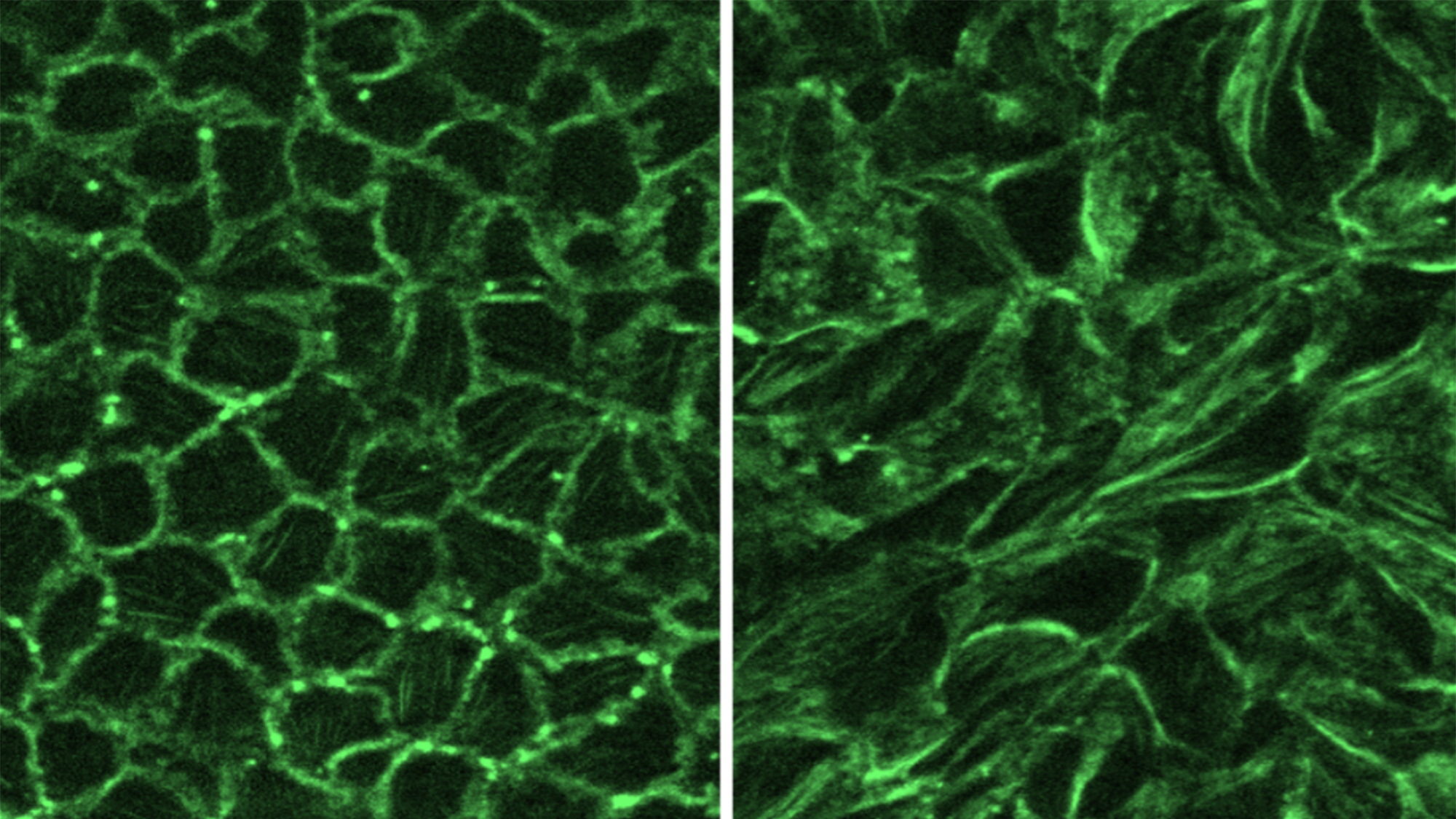
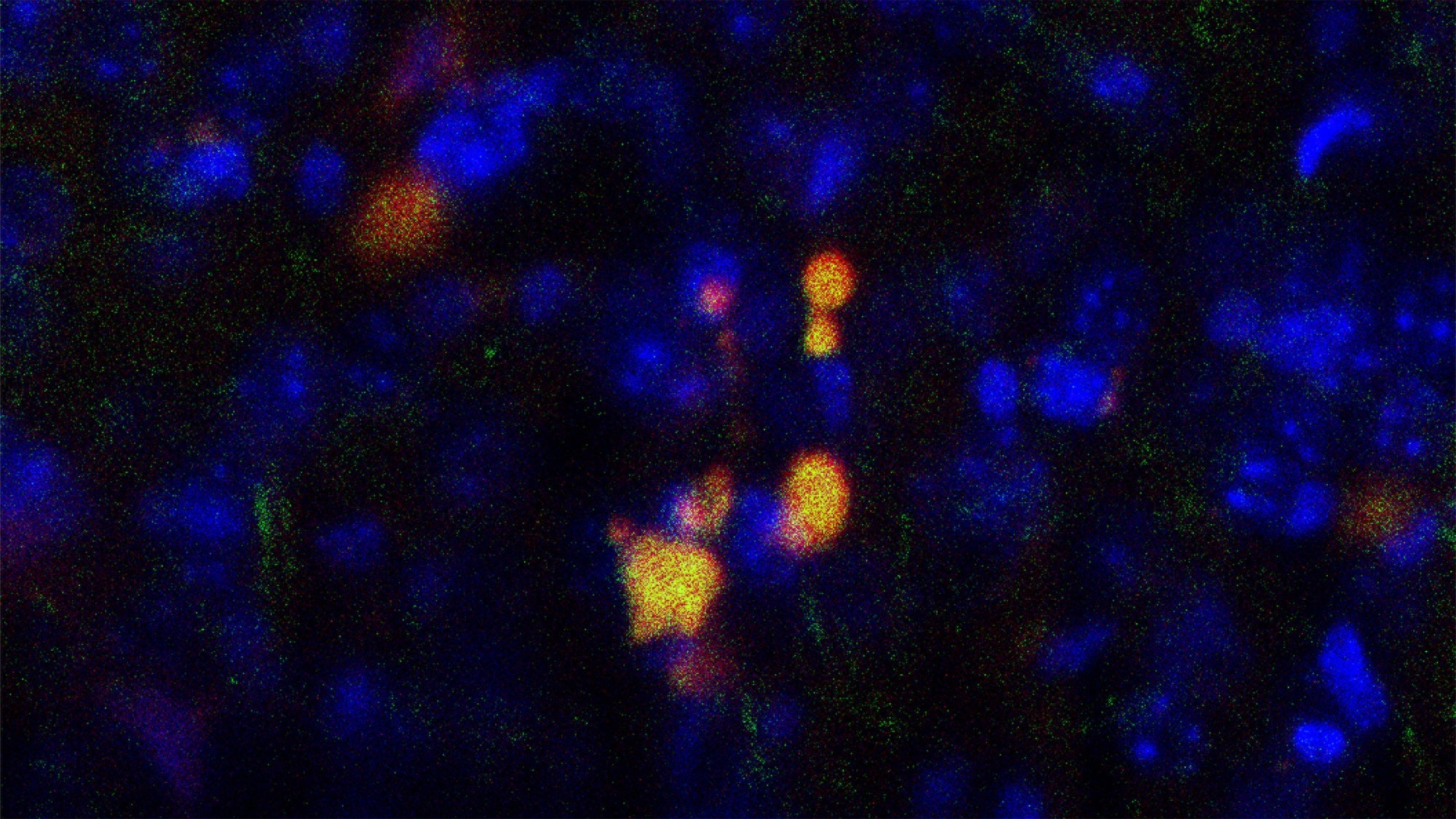
To advance understanding of mitochondrial ROS (mROS) generation—and its health consequences—the researchers zeroed in on the liver, a central organ for glucose and lipid homeostasis that has never been studied in detail in terms of mROS production. The study explored all possible sources of mROS in the liver from both lean and obese mice. It found that the obese mice’s livers failed to produce proper amounts of coenzyme Q, a molecule essential to energy production. This defective coenzyme Q metabolism drives an unusual process called reverse electron transport (RET) that occurs in an enzyme called complex I, causing mitochondria to increase generation of ROS and, consequently, disrupt metabolism. The researchers observed similar alterations in coenzyme Q metabolism when analyzing the genes and measuring coenzyme Q ratios in people with another metabolic disorder, fatty liver disease.
Prior studies had shown that eliminating ROS using broad antioxidants hasn’t improved outcomes in conditions like obesity, insulin resistance, and cardiovascular disease. The new study shifts the paradigm, said lead author Renata Goncalves, research associate in the Department of Molecular Metabolism.
“Instead of broad, unselective interventions, we systematically investigated the sources of mROS, and now know precisely where the excess is coming from and why,” she said. “We’ve reframed the problem from a generalized to a site-specific phenomenon, so in the future, instead of broad-spectrum antioxidants, a tailored cocktail of compounds could be developed to effectively, safely reduce mROS, either through decreasing RET, increasing coenzyme Q levels, or both to treat metabolic diseases including type 2 diabetes.”
Other Harvard Chan co-authors included Zeqiu Wang, Jillian Riveros, Gunes Parlakgul, Karen Inouye, Grace Lee, Jani Saksi, Sheng Hui, Ana Arruda, and Isabel Graupera.
The study was funded by the Barth Syndrome Foundation, the National Institutes of Health (grants DK123458, HL148137, P30DK127894, and R01DK128168), and the Juvenile Diabetes Research Foundation (grant 2-SRA-2019-660-S-B).
“Ubiquinone deficiency drives reverse electron transport to disrupt hepatic metabolic homeostasis in obesity,” Renata L.S. Goncalves, Zeqiu Branden Wang, Jillian K. Riveros, Gunes Parlakgul, Karen E. Inouye, Grace Yankun Lee, Xiaorong Fu, Jani Saksi, Clement Rosique, Sheng Tony Hui, Mar Coll Loperena, Ana Paula Arruda, Shawn C. Burgess, Isabel Graupera, Gökhan S. Hotamisligil, Nature, May 28, 2025, doi: 10.1038/s41586-025-09072-1
Visit the Harvard Chan School website for the latest news, press releases, and events from our Studio.
For more information:
Maya Brownstein
mbrownstein@hsph.harvard.edu
###
Harvard T.H. Chan School of Public Health is a community of innovative scientists, practitioners, educators, and students dedicated to improving health and advancing equity so all people can thrive. We research the many factors influencing health and collaborate widely to translate those insights into policies, programs, and practices that prevent disease and promote well-being for people around the world. We also educate thousands of public health leaders a year through our degree programs, postdoctoral training, fellowships, and continuing education courses. Founded in 1913 as America’s first professional training program in public health, the School continues to have an extraordinary impact in fields ranging from infectious disease to environmental justice to health systems and beyond.