A midwife and an obstetrician meet at orientation…

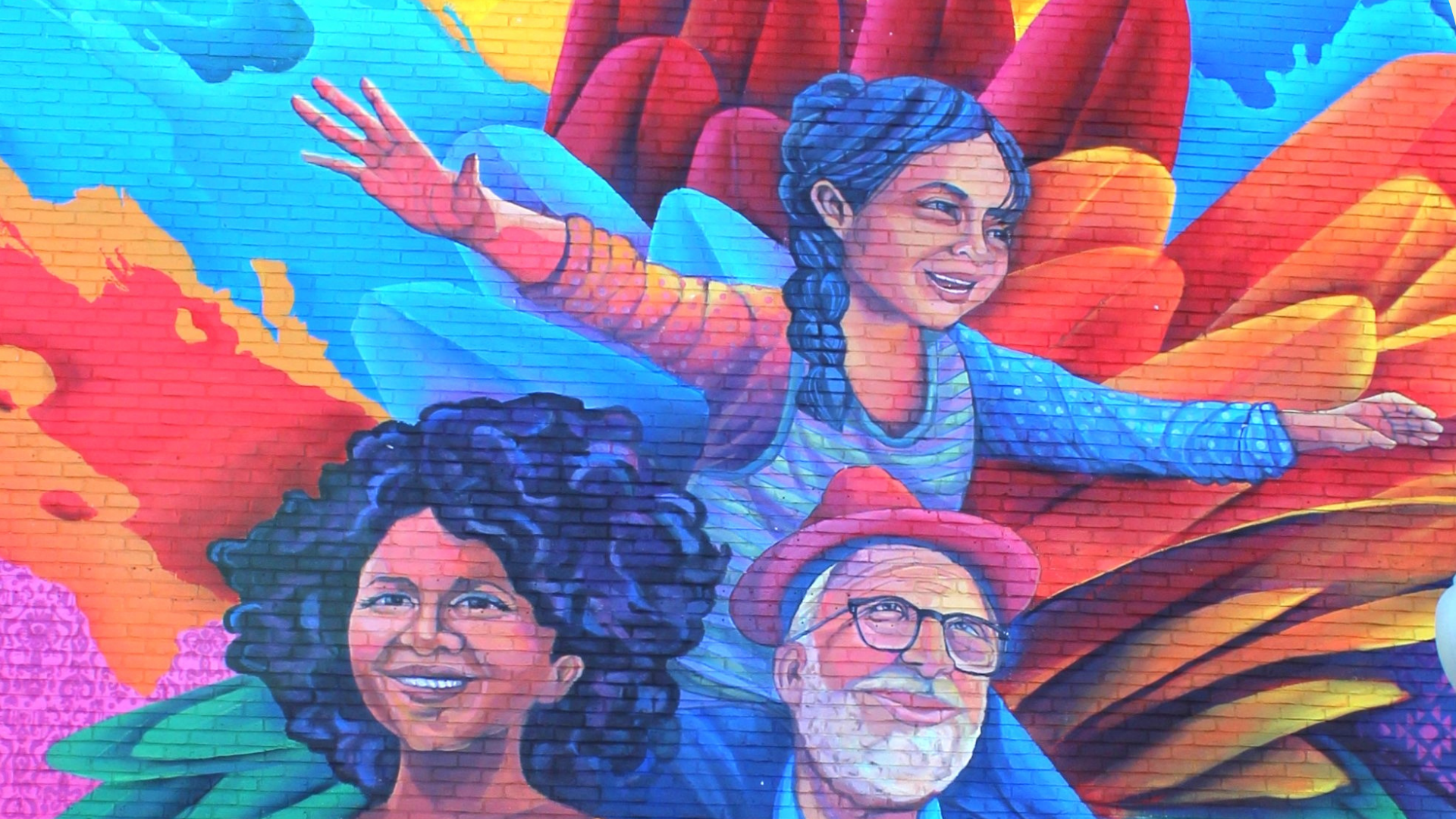
Cathy Han, Ariel Bernstein, and Dr. Bameka Agery at the Busoga Health Forum office in Jinja, Uganda
Ariel and I met during an orientation week at Harvard T.H. Chan. She is a midwife from Maine, and I am an obstetrician from California. We were both interested in volunteering in Uganda, a country with a high maternal mortality rate of 284 maternal deaths per 100,000 women, compared to 21 per 100,000 in the United States. I had experience with implementing best practices in hospital settings and she had experience with delivering babies in low-resource areas. We quickly realized that our skills would complement each other.
In the fall, we partnered with two Ugandan physicians and the Busoga Health Forum, a community organization committed to improving health outcomes in the Busoga region of eastern Uganda. Their mission is “to rally Busoga professionals to use evidence to engage community, government and partner action for better health of children, youth, women and men in Busoga.” By utilizing their Whats App group, they successfully mobilized forty midwives to participate in our simulation trainings that were to take place at Jinja Hospital. We used the funds from our Rose Service Learning Fellowship award to provide transportation, lunch, anatomical models, and training manuals for the midwives.
On our first day in Jinja, Uganda, we got some curious looks on our way to the hospital. Ariel and I each rode on the back of a motorcycle taxi or “boda boda,” carrying a mannequin in a large backpack. Ariel laughed at how tightly I was gripping onto my driver and told me to lighten up so he could breathe. As we set up our materials in the hospital library, we were relieved as the first group of midwives arrived. In their dresses and heels, they looked like they could be going to church. They told us it was not every day that they had visitors from Harvard!. They were used to didactic lectures but had never done simulation drills with role playing and mannequins.
Trip on the back of a boda boda Bike
Ariel and I took turns leading the simulation drills and played to our strengths. Ariel had more experience with vaginal breech deliveries and demonstrated the maneuvers with the mother-baby model. I reviewed the protocols for postpartum hemorrhage and pre-eclampsia that my California hospital in California had implemented as “best practices.” We soon discovered that some of the midwives were natural teachers. Sister Betty made us laugh as she dramatically wailed as if she were in labor. Sister Phiona showed us how to improvise an intrauterine balloon device from an inexpensive catheter and a glove.

On the third day, we visited Labor and Delivery and the midwife on duty unexpectedly recruited us to help for a few hours. She handed us gloves and Ariel delivered a baby 30 minutes later. I resuscitated two babies who were having trouble breathing. There were no delivery beds or drapes; women gave birth on top of a rubber mattress covered by a black plastic garbage bag. The unit had one bulb syringe to suction all the babies. One woman had a hemorrhage, but the midwife couldn’t draw up oxytocin because they had run out of syringes. I asked if we could give her tranexamic acid or methergine or a blood transfusion, but none of those were available.
After we left the hospital, I told Ariel, “I’m so glad you’re here…because it would be hard to explain what this was like to anyone in the U.S.” We had not expected the conditions to be this dire in a large regional hospital. We now had even more respect for the midwives’ ability to practice with such limited resources.
In California, I’ve delivered 3000 babies over 15 years and have never experienced the tragedy of losing a mother. In Jinja, one of the midwives gave us a tour and pointed out a patient who had been transferred to the hospital after a significant postpartum hemorrhage at home. Sister Joselyn said “she’s going into shock… I’m not sure she’s going to make it…and there’s no blood available.” Ariel and I asked if we should donate blood, but we had the wrong blood type. It felt strange and terrible not to be able to do anything. We asked Sister Joselyn about the patient the next morning and she just shook her head slowly.
Ariel and I helped each other process the trauma of not being able to save a woman from dying in childbirth. We contemplated the toll it must take on the midwives. Our training seemed insignificant compared to the major challenges they face. What saved us from despair was reading the midwives’ comments on their post-training surveys. They universally reported that they had learned skills and had more confidence in their abilities.
Ariel and I have thought about how to make the training in Uganda sustainable. Our goal is to return in the summer and train a few of the midwives to become trainers themselves. We felt incredibly lucky to be able to teach as a team and plan to return together. Despite the lack of resources, we hope to empower the midwives with the tools of knowledge and confidence.
Ariel interviewed on podcast, shares about her time in Uganda.