Harvard China Health Partnership
The Harvard China Health Partnership (HCHP) is a school-wide initiative dedicated to advancing scholarship on China’s health system, evaluating and designing health policy interventions, and improving health care in China.
665 Huntington Ave
Building 1, Room 1210
Boston, MA 02115

Analysis of Provider Payment Reform on Advancing China’s Health (APPROACH)
The “Analysis of Provider Payment Reform on Advancing China’s Health” (APPROACH) project evaluated a social experiment that modified the provider payment system at county-level hospitals. In collaboration with the Government of Guizhou–one of the poorest provinces in China with a large rural population–we launched a social experiment in 28 counties of Guizhou in from 2016 to 2018. Another 28 counties served as control counties, which allowed us to evaluate data from hospital information systems, New Cooperative Medical Scheme (NCMS) claims records, and two hospital surveys.
Background
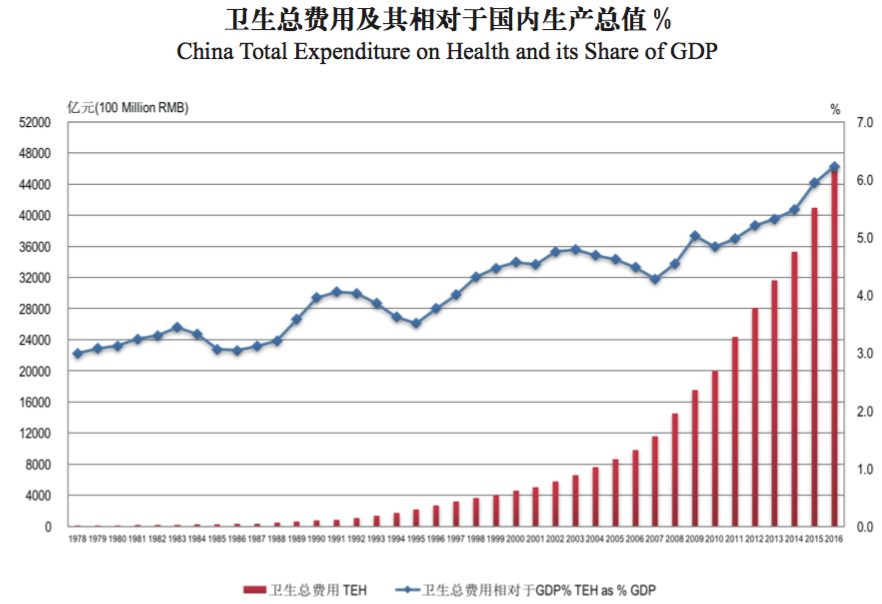
Health care expenditure in China has been increasing rapidly, both in real terms and as a percentage of GDP, as is shown in the figure below. While various health care schemes have covered over 95 percent of the population by the end of 2011, the financial protection they offer are insufficient, leaving many households vulnerable to catastrophic health expenditure.
One root cause of the increase in expenditure is misaligned incentives faced by health care providers. They are paid by fee-for-service (FFS) according to a fee schedule that overpays for drugs and high-tech diagnostic tests and underpays for basic services, such as consultations. As a result, both overprovision (of profitable drugs and tests) and underprovision (of unprofitable basic services) are common, leading to cost escalation and inappropriate treatments.
The Chinese government has acknowledged this problem and placed great importance on provider payment reform in the latest Five Year Plan. Specifically, the plan calls for a shift from FFS to prospective provider payment methods (PPM), such as global budget, capitation and case-based payments.
In collaboration with the Government of Guizhou (one of the poorest province with a large rural population in western China), we launched a social experiment in Guizhou in 2016. Our intervention is targeted at the PPM for inpatient services of the New Cooperative Medical Scheme (NCMS). It changes the PPM from FFS to a mixed payment method combining a disease-based global budget and pay-for-quality (hereafter GB+P4Q) for county hospitals. Under this method, county hospitals receive a prospective budget based on the size of the enrolled population in NCMS at the beginning of the year, with 30 percent of the budget withheld and disbursed based on performance assessment biannually. The capitation rate is calculated to cover county hospital expenditure and a portion of out-of-county expenditure based on spending over the last three years.
Policy Intervention
We designed the global budget in a way that incentivized county hospitals to build their capacities and play a gate-keeping role to not refer patients to out-of-county hospitals for health conditions that they can treat. Specifically, the budget was calculated as follows.
If county hospitals referred patients to out-of-county hospitals for health conditions that they are capable of treating, expenditure incurred at these higher-level hospitals would be paid from the county hospital’s budget. To align incentives on the demand side, the NCMS reimbursement rates for municipal hospitals were adjusted to be lower than that for county hospitals. Reimbursement rates at these higher-level hospitals without referrals were also reduced to only half of that with referrals.
Quality performance indicators consisted primarily of process of care measures. They fall into two sets: non-disease specific measures and disease-specific measures. Table 1 gives the list of non-disease specific measures and their sources and formulas.
For disease-specific measures, after an examination of the inpatient data, the following diseases were identified as focal areas: pneumonia, chronic obstructive pulmonary disease (COPD), ischemic cerebral infarction, and acute myocardial infarction (AMI). Using the US Hospital Quality Alliance framework (HQA) and UK Advancing Quality framework as references, a subset of indicators were selected as disease-specific measures.
Each hospital received a score based on their quality improvements from the previous year.
Study Design
Guizhou province was selected as the study site as it is one of the most underdeveloped provinces in China with a large rural population. Of all the districts and counties in Guizhou, those where NCMS has a low coverage rate or is administered by the Department of Human Resources and Social Security, and those with pre-existing payment reform programs, were excluded from the study. The study sites should be representative of China’s western regions and the lower-income areas of the central region. Figures 1 and 2 show the location of Guizhou province and 28 intervention counties in Guizhou respectively.

Figures 1 and 2 shows the location of Guizhou province and 28 intervened counties in Guizhou respectively.

The study adopted a matched-pair cluster randomization strategy. A total of 56 counties were eligible for the randomization and matched on a vector of county-level characteristics on population, economics, and health care. For each set of matched counties, treatment was randomly assigned within pair-wise match.
During 2014-2015, the interventions were first piloted in 2 counties in order to develop detailed SOPs. The real interventions were rolled out since 2016 across two waves (the first wave started at the beginning of 2016, and the second wave started at the beginning of 2017). The selection of interventions for 2016 vs 2017 implementation was random.
The intervention is a government policy change to the provider payment system at the county-level hospitals. The study hospital sample includes all county-level hospitals in the study counties—intervention and control. The study population includes all NCMS enrolees in the intervention and control counties, covering >95% of all population in the counties.
Indicators used in this study include Internal Management, Contextual and Mediating Factors, and Quality.
Outcome variables are obtained from county hospital discharge data and NCMS claims records, including information on health care expenditure, insurance reimbursement, out of pocket payment, expenditure for drugs and diagnostic tests, and length of stay.
Research Products
- Lin, Xiaojun, Weiyan Jian, Winnie Yip, and Jay Pan. “Perceived competition and process of care in rural China.” Risk Management and Healthcare Policy (2020): 1161-1173. doi: 10.2147/RMHP.S258812