Apple Women’s Health Study
The Apple Women’s Health Study is the first long-term research study of this scale and scope that aims to advance the understanding of menstrual cycles and their relationship to various health conditions.
COVID-19 vaccines and menstrual cycles
The Apple Women’s Health Study explores the relationship between menstrual cycle length and COVID-19 vaccination

JULY 2022: Menstrual cycles are considered by many medical professionals as a window into overall health. Each person’s menstrual cycle pattern can be affected by changes in behavior, medical conditions, or habits. However, there is not a lot of research about the possible connection between menstrual cycle changes and vaccination.
Some people reported through the United States Vaccine Adverse Event Reporting System (VAERS) that they experienced changes to their menstrual cycles after getting the COVID-19 vaccine1,2. These reports led us to ask about menstrual cycle patterns, and how they may have changed for participants in the Apple Women’s Health Study after they were vaccinated.
Vaccines provide instructions to your body on how to protect you from getting an infectious disease. Messenger RNA (mRNA) vaccines “use mRNA created in a laboratory to teach our cells how to make a protein—or even just a piece of a protein—that triggers an immune response inside our bodies”3. Viral vector vaccines “use a modified version of a different virus (a vector virus) to deliver important instructions to our cells” 4,5. Vaccines trigger an immune response in your body which produces antibodies6. It is normal to experience mild side effects during the immune response.
Thanks to participants who filled out the COVID-19 Vaccination Update survey, we were able to look at over 125,000 menstrual cycles, evaluate changes to these cycles, and understand the association of these changes with recent vaccination. We found that participants experienced slightly longer menstrual cycles for cycles in which they received a COVID-19 vaccine. Participants’ cycles typically returned to pre-vaccination lengths the cycle after getting a vaccine. See the figures below to learn more.
Our preliminary insights support other research7 and emphasize that menstrual cycle changes associated with COVID-19 vaccination are small and temporary and should not discourage people from getting vaccinated.
Majority of participants reported being vaccinated against COVID-19
In this analysis, we included data from 9,652 participants that filled out the COVID-19 Vaccination Update survey through February 2022 and self-reported menstrual cycles. Of respondents, 8,486 participants (88%) reported that they received a COVID-19 vaccine, while 1,166 (12%) did not. In comparison, 77% of women in the U.S. over the age of 18 had received a COVID-19 vaccine by February 20228,9.
Of the participants that were vaccinated, 55% received Pfizer-BioNTech, 37% received Moderna, and 7% received Johnson & Johnson/Janssen (J&J). The Pfizer-BioNTech and Moderna vaccines are mRNA COVID-19 vaccines, and the J&J vaccine is a viral vector vaccine. In this analysis, we will refer to the vaccines by their vaccine type.
This analysis looks at the primary series of COVID-19 vaccination, which is the first round of vaccination, as recommended by the Centers for Disease Control and Prevention (CDC), to be fully vaccinated10. The primary series for the mRNA vaccines is two doses; the primary series of the viral vector vaccine is one dose. While this analysis does not look at boosters, to be up to date on your COVID-19 vaccination, the CDC recommends that you receive a booster vaccine when eligible11.
Small and temporary changes in menstrual cycles post vaccination
We found that the small and temporary change in average menstrual cycle length for cycles in which a vaccine dose was received was within the range of natural cycle variability. For the participants included in this analysis, regardless of vaccination status, it was common to experience menstrual cycles that varied up to 4.2 days from cycle to cycle. This is aligned with scientific research about how it is normal for menstrual cycles to vary and change from month to month12.
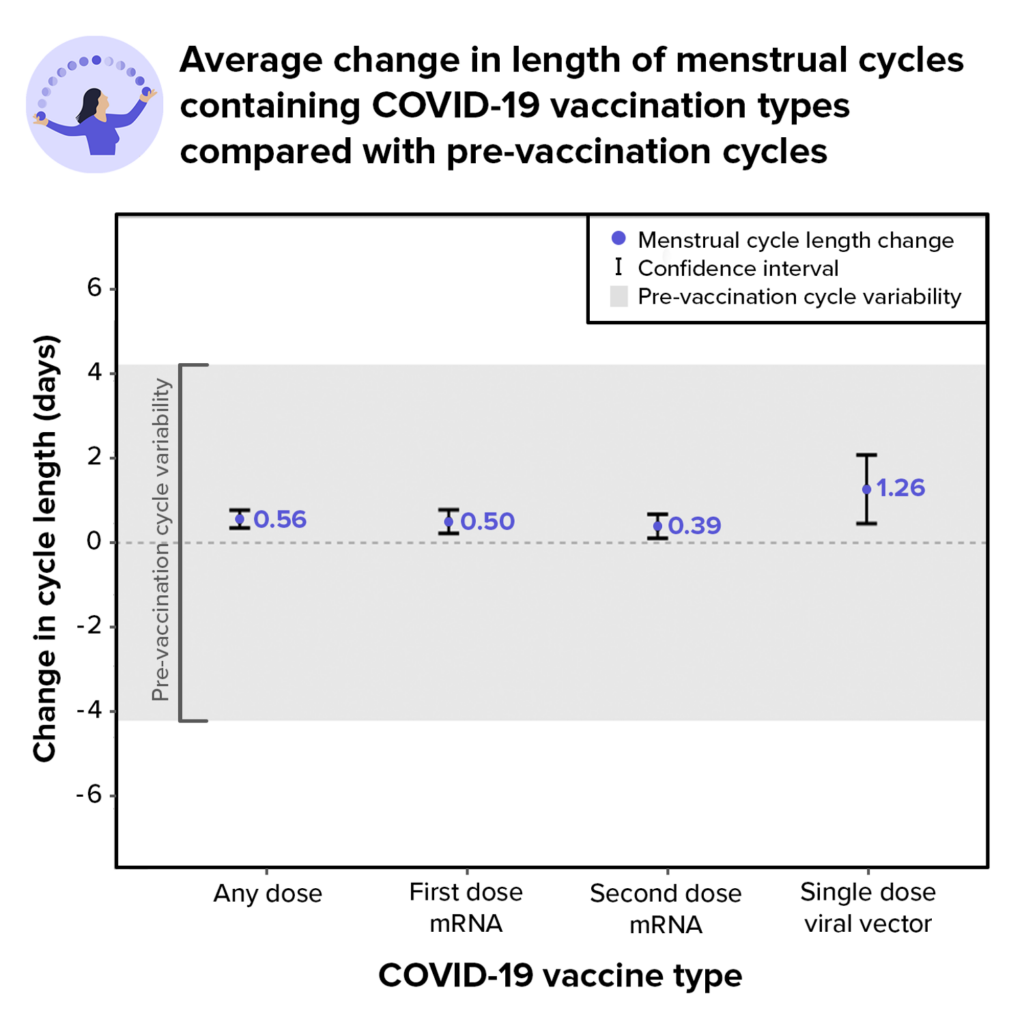
We conducted a within-person analysis, meaning that we looked at differences in menstrual cycle lengths for individual participants, not differences between participants. On average across all participants that received a vaccine dose, their menstrual cycle increased by about half a day, specifically 0.56 days.
In comparison with pre-vaccination menstrual cycles, cycles containing the first dose of an mRNA COVID-19 vaccine increased in length by 0.50 days, and cycles containing the second dose of an mRNA COVID-19 vaccine increased in length by 0.39 days. Cycles in which a viral vector vaccine was administered were, on average, 1.26 days longer than the pre-vaccination cycles.
These menstrual cycle changes are illustrated in the chart below. On the chart, a longer menstrual cycle is noted by a measurement above the zero line, whereas a shorter menstrual cycle is noted below the zero line. The area shaded in grey corresponds to the range of pre-vaccination cycle variability.
While there was a small change in menstrual cycle length for cycles in which a COVID-19 vaccine was administered, our statistical models found no evidence of a difference in length of menstrual cycles following vaccination. The chart below shows that changes to menstrual cycle length did not persist over time, with average menstrual cycle length returning to pre-vaccination average length in the following cycle.
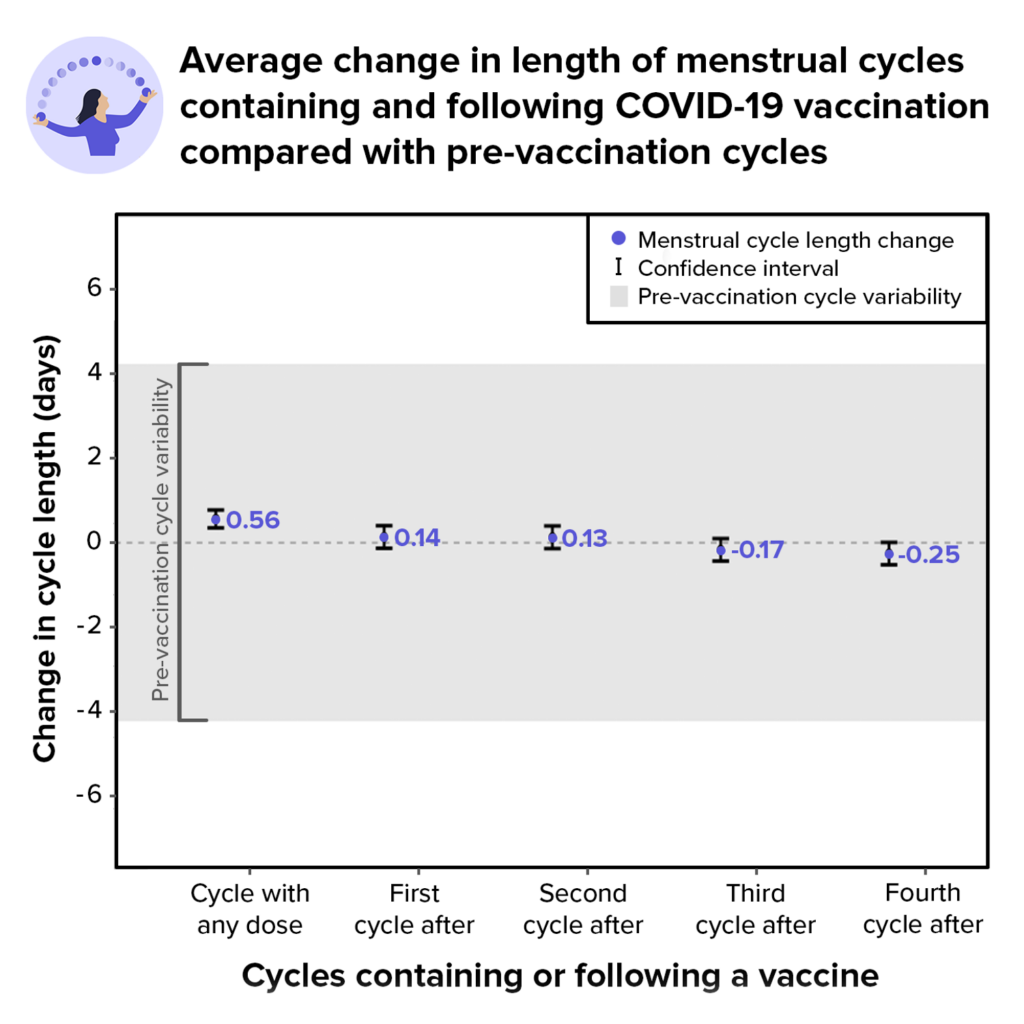
The small, less than half day change in menstrual cycle length observed in cycles containing a COVID-19 vaccine dose did not persist for the four cycles following a vaccine dose. In a future scientific publication, our team will explore the association between vaccination timing by day of the menstrual cycle (before and after ovulation) and impacts on menstrual cycle lengths.
Importance of studying menstrual cycle changes
Our preliminary insights confirm that changes to menstrual cycles associated with COVID-19 vaccination are small and temporary, and within the range of pre-vaccination variability. We found that the menstrual cycle in which a vaccine was administered was about half a day longer in comparison with pre-vaccination cycles, and most cycles returned to pre-vaccination average length by the following cycle.
COVID-19 vaccines are safe and effective in preventing infection and severe COVID-19 illness13. Even with its strong protection against severe illness and even death, it is important to understand side effects of the vaccines, and this research affirms the importance of studying menstrual cycles and their relationship to overall health – including the immune system14.
Our team looks forward to continuing our work to better understand the relationship between lifestyle factors and menstrual health. Thank you to participants for contributing important information to the Apple Women’s Health Study.
More information on Apple Research App & Privacy
- Centers for Disease Control and Prevention (CDC). CDC Wonder. About The Vaccine Adverse Event Reporting System (VAERS). Accessed online in May 2022.
- CDC. CDC Wonder. The Vaccine Adverse Event Reporting System (VAERS) Results Form. Accessed online in April 2022.
- CDC. Understanding mRNA COVID-19 Vaccines. Accessed online in May 2022.
- CDC. Johnson & Johnson’s Janssen COVID-19 Vaccine: Overview and Safety. Accessed online in May 2022.
- CDC. Understanding Viral Vector COVID-19 Vaccines. Accessed online in May 2022.
- World Health Organization (WHO). Side Effects of COVID-19 Vaccines. Accessed online in May 2022.
- Edelman A, Boniface ER, Benhar E, et al. Association Between Menstrual Cycle Length and Coronavirus Disease 2019 (COVID-19) Vaccination: A U.S. Cohort. Obstet Gynecol. Published online January 5, 2022. doi:10.1097/AOG.0000000000004695.
- CDC. COVID Data Tracker. Atlanta, GA: US Department of Health and Human Services, CDC. Published March 28, 2020. Accessed April 29, 2022. https://covid.cdc.gov/covid-data-tracker
- U.S. Census Bureau. 2019 Population Estimates by Age, Sex, Race and Hispanic Origin. Published June 25, 2020. Accessed April 29, 2022. https://www.census.gov/newsroom/press-kits/2020/population-estimates-detailed.html
- CDC. Stay Up to Date with Your COVID-19 Vaccines. Accessed online in May 2022.
- CDC. COVID-19 Vaccine Boosters. Accessed online in May 2022.
- Harlow SD, Ephross SA. Epidemiology of menstruation and its relevance to women’s health. Epidemiol Rev. 1995;17(2):265-286. doi:10.1093/oxfordjournals.epirev.a036193
- CDC. Safety of COVID-19 Vaccines. Accessed online in May 2022.
- Chrousos GP, Torpy DJ, Gold PW. Interactions between the hypothalamic-pituitary-adrenal axis and the female reproductive system: clinical implications. Ann Intern Med. 1998;129(3):229-240. doi:10.7326/0003-4819-129-3-199808010-00012