One thing everyone should know about innate immunity
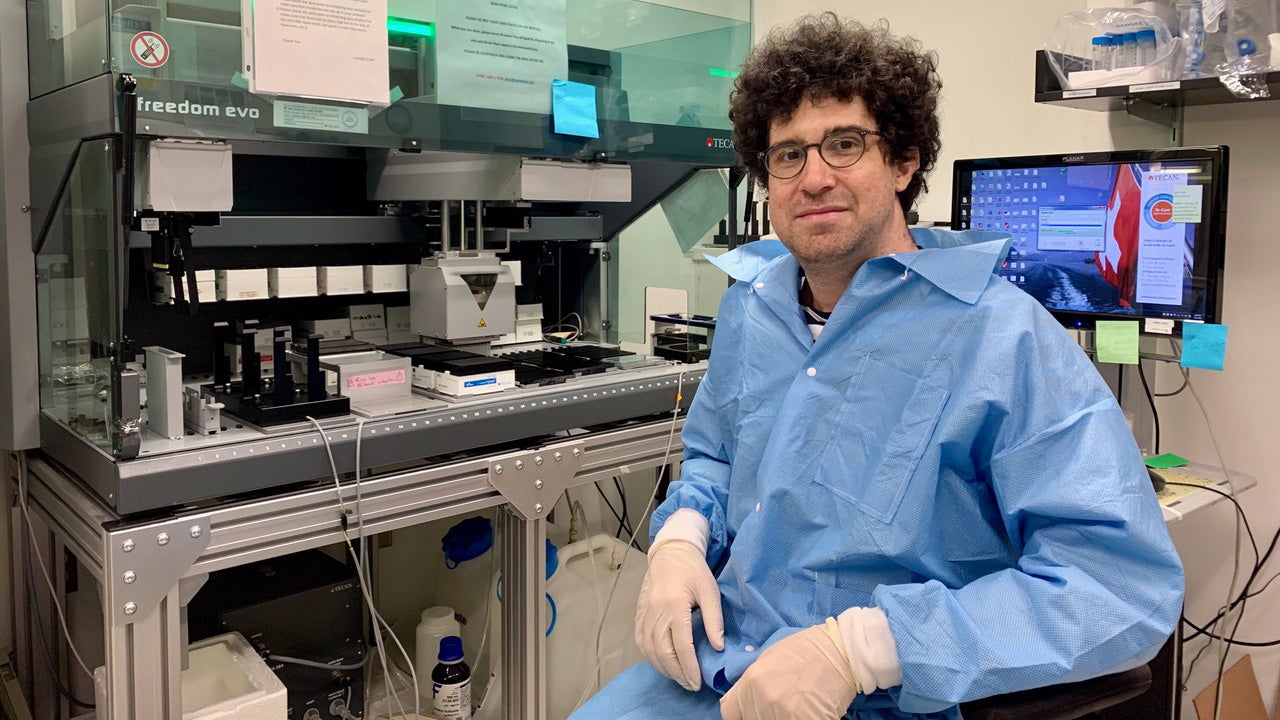
Jérémie Le Pen, assistant professor of immunology and infectious diseases at Harvard T.H. Chan School of Public Health, shares one thing everyone should know about the innate immune system, our body’s first line of defense against infection: We can harness it to help keep people from becoming seriously ill.
Have you ever wondered why, in the same household, one person might catch a bad case of the flu, while others show no symptoms? Part of the answer lies in our genes—some of us are more vulnerable or resistant to viral infections from birth.
As part of innate immunity—the immunity we are born with—our cells naturally produce powerful antiviral molecules called interferons, which fight viruses from the very beginning of an infection. An infected cell secretes interferons as a distress signal, which are then received by surrounding cells. In response, those neighboring cells produce antiviral proteins, including some that block the virus from entering them—essentially shutting the door before the virus can get inside and start multiplying.
But some people are born with genetic mutations that prevent them from making or responding to interferons. For example, early in the COVID-19 pandemic, my colleagues and I analyzed the genomes of children hospitalized with pneumonia and found that about 10% had inherited mutations in genes critical for innate immunity.
Another issue is that some people develop autoantibodies—immune proteins that mistakenly target and block their own interferons. In one study, we estimated that up to 15% of patients with severe COVID-19 carried these autoantibodies.
The situation is a bit like diabetes: just as people with diabetes can’t produce or respond to insulin, some individuals can’t produce or respond to interferons. In that sense, certain cases of severe viral infections like flu or COVID-19 aren’t just infectious diseases—they can also be viewed as chronic conditions linked to inherited, genetic defects in immune function.
With current technology, we can identify people with mutations that may make them more susceptible to viruses—and we can then protect them by giving them priority access to treatment when when vaccines or antivirals hit the shelf. In the future, we may be able to go further: restoring the faulty genes, or compensating with preventive medication, so that people never become seriously ill in the first place.
The more we understand how interferons work at a molecular level, the better we can harness this knowledge to design new antiviral therapies inspired by nature—and ensure that everyone’s innate immune system is equipped to fight back.