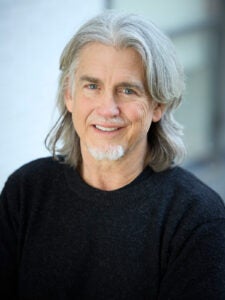
John Quackenbush, Henry Pickering Walcott Professor of Computational Biology and Bioinformatics at Harvard T.H. Chan School of Public Health and chair of the School’s Department of Biostatistics, does groundbreaking research that uses massive gene datasets to explore how diseases progress, particularly cancer. Here, he explains the origins of his work, the advances that have been made, and the crucial support that federal funding provides.
Q: Tell us about your team’s research and how it evolved.
A: In 2001, the Human Genome Project provided a catalog of the 25,000 genes encoded in the genome. Researchers worldwide have been exploring that catalog to learn more about the connection between the genes we carry and the ways that diseases develop, progress, and respond to therapy.
Most people know our genes determine our traits. People at first thought that if we could determine how your genome is different than my genome, we’d be able to understand why we each exhibit different traits—including traits that determine our state of health and the characteristics of disease we develop.
But we quickly realized that genomic differences are only one part of the story. Think of it this way: Your brain cells and your liver cells have exactly the same genome, the same DNA, yet brain cells make neurotransmitters while liver cells make digestive enzymes. In the same way, we see different manifestations of what’s in the genome in healthy and diseased states.
As early as 2005, my research team started to approach the genetic catalog as more of a parts list that tells us what could make up a cell—but not how everything is put together. Years of biological research had told us that there were processes in which about 1,600 proteins in cells control the 25,000 genes encoded in the genome, turning those genes on and off. But teasing out which of the 40 million possible “controls” were active in each biological state—for example, in both healthy and diseased cells—and seeing how those controls change as healthy cells transform into disease cells was impossible.
In 2012, we made a conceptual leap and developed a method called PANDA that, for the first time, solved the problem. PANDA was able to use data on which of the 25,000 genes are turned on or off in specific biological samples to “reverse engineer” the control networks active in each cell type. PANDA let us move from observing “what” was happening with gene expression to explaining “why” and “how” it was happening—for the first time, the control mechanisms that are active, encompassing all of the genes in the genome, could be learned from data and compared between biological states.
This was a revolutionary advance that allowed us to begin to tease apart what makes cells different and why different processes of gene regulation occur in different cell types. Even we were surprised how effective these methods were in finding changes in the regulatory control mechanisms that, for example, transform “normal” healthy cell function to perturbed functions in disease states.
We’ve since continued to improve our models and have been using them to explore previously unanswerable questions regarding the disease process, particularly in cancer. For example, we’re exploring why so many diseases manifest differently in males and females. Our gene regulatory network approach is a crucial linchpin in helping us understand how to treat cancer in a better and more personalized way.
Q: How is this new approach advancing novel possibilities for cancer prevention and treatment?
A: I can give you two examples. One involves exploring colon cancer to understand how and why the disease manifests differently in males and females—males have a greater risk of colon cancer but respond better to chemotherapy. We built separate gene regulatory network models in the two sexes and compared them. We found that the sexes differ in how cells regulate immune processes, which helps explain the differences in risk. But we also discovered that females regulate drug transport and metabolism differently, which suggests some potential ways that we may be able to alter their tumors’ susceptibility to chemotherapy. We are now using those tools with a colleague studying breast cancer and she has been amazed that nearly every chemotherapy treatment option our methods have identified seems to work in mouse models. This is unprecedented.
We are also asking questions about the dynamic processes about how cancer develops over time. Most people talk about health and disease as if they are discrete things that are separate from each other. But you don’t just wake up with cancer. It emerges from a disease process that exists along a continuum. We have developed a new method called PHOENIX that can, for the first time, create models of how the regulation of all 25,000 genes changes between healthy and cancerous cells. We are now in the process of determining exactly where key changes in gene regulation occur that drive healthy cells to transform into cancer cells, with the goal of finding drugs that can stop the process in its tracks—before cancers become killers. My team was very proud when the National Cancer Institute named PHOENIX one of the most important advances of 2024.
Q: How has federal research funding contributed to your work?
A: All of my research has been funded by grants—nearly all from the National Institutes of Health (NIH). I got my first NIH grant in 1992, allowing me to transition from a PhD in theoretical physics to being a biomedical researcher. If I do say so myself, that was a good investment, and I have been funded ever since. Getting grants isn’t easy and you really have to propose good ideas that address important unanswered questions.
NIH funding has allowed me to write more than 340 scientific papers that have collectively been cited by my peers over 100,000 times. I’ve used this funding to attract students and postdoctoral fellows who, after training with me, are professors at some of the top universities around the world or are leaders in pharmaceutical and biotech companies. And my team and I have developed software tools that make our methods available to anyone around the world free of charge. But most importantly, the advances that have been enabled by my work are entirely dependent on federal grants. Solving the mysteries of human gene control is incredibly hard and it has taken us a long time to get where we are. But along the way, we have gained valuable, practical insight into cancer and other diseases. None of this would have been possible without funding from the NIH.
Aside from the direct funding that has supported me and my team, NIH grants come with funding for so-called “indirect costs”—costs for facilities and administration. The Trump administration has proposed cutting these dramatically and the effects of that would be devastating. Funding for indirect costs covers things like lab space, equipment, computing resources, and administrative support. Here at Harvard, this funding has supported the large-scale computing facilities that allow us to model genome-wide gene regulatory networks. It allows us to comply with federal regulations about securely analyzing data from human subjects. It enables us to provide detailed accounting of our work so that I can demonstrate, to the last dollar, how I am using the research grants I receive for the public good by doing the work I was contracted to do. And it allows me to have the administrative support to apply for new research grants that will allow me take on the next stage in my disease research.
What a lot of people may not realize is that the funding for indirect costs supports shared resources across all of our research faculty. It is not just a gift to Harvard; it reflects the substantial cost of doing research for the public good and they are costs that we can’t bill directly to the government. If Harvard were a company, we’d build all of these costs into our grant proposals directly. Indirect costs were introduced into the grant process by the government as a way of sharing costs efficiently between academic institutions and the government.
Q: Recently, you and other Harvard researchers received notices that your grants were being terminated. What will be the impact on your work and that of other researchers across the U.S.?
A: On the afternoon of Thursday, May 15, I was flying to my niece’s wedding. I was over Lake Michigan when my e-mail started blowing up as the mass terminations of Harvard’s federal research grants were rolled out. Even though I knew it was coming, my heart sank. The research funding supporting what I had spent 33 years building had vanished. That means that, absent other funding sources, my research stops. What that means is that the work I have done and the progress we’ve made will be stopped in its tracks along with the leads we have for improving how cancer is treated. I also learned that all four NIH training grants—which support our PhD students—were terminated.
Beyond my own work, there is a human cost. In my research group, we have people with expertise built up over years. If they fall out of the field, it will be hard to bring them back. My team of postdoctoral fellows may be without support and so many are already looking for other positions—including overseas. PhD students learn by doing an apprenticeship and if we lose our ability to train students—which comes from federal training and research grants—the next generation of quantitative scientists in biomedical research is going to be decimated.
And this extends across Harvard and beyond. People who are at the top of the field are going to go where there is funding for health and biomedical research. I’ve heard from colleagues and collaborators overseas. They’re looking at what’s happening in the U.S. and are already starting to recruit our scientists. I regularly hear from colleagues who are looking for positions and those outside the country who are looking to recruit.
Science in the U.S. has excelled because we’ve brought the best and the brightest from around the world here. We don’t want to give up that advantage and have outstanding scientists go elsewhere. If we don’t maintain the infrastructure here around research and education, it will put the U.S. and its decades of leadership in health and biomedical research at risk. We want to keep American preeminence in these areas and to do that, we have to make the kind of investments that we’ve learned to make effectively over decades.
We do this work because we love the thrill of discovery and the rewards of training future scientists. We stay in academic science because we have the freedom to share what we do widely with others for the benefit of humankind. But doing science for the public good relies on the federal government’s investment in supporting research and with it, improved health for all Americans.