Coronavirus (COVID-19): Press Conference with Barry Bloom and William Hanage, 12/16/20
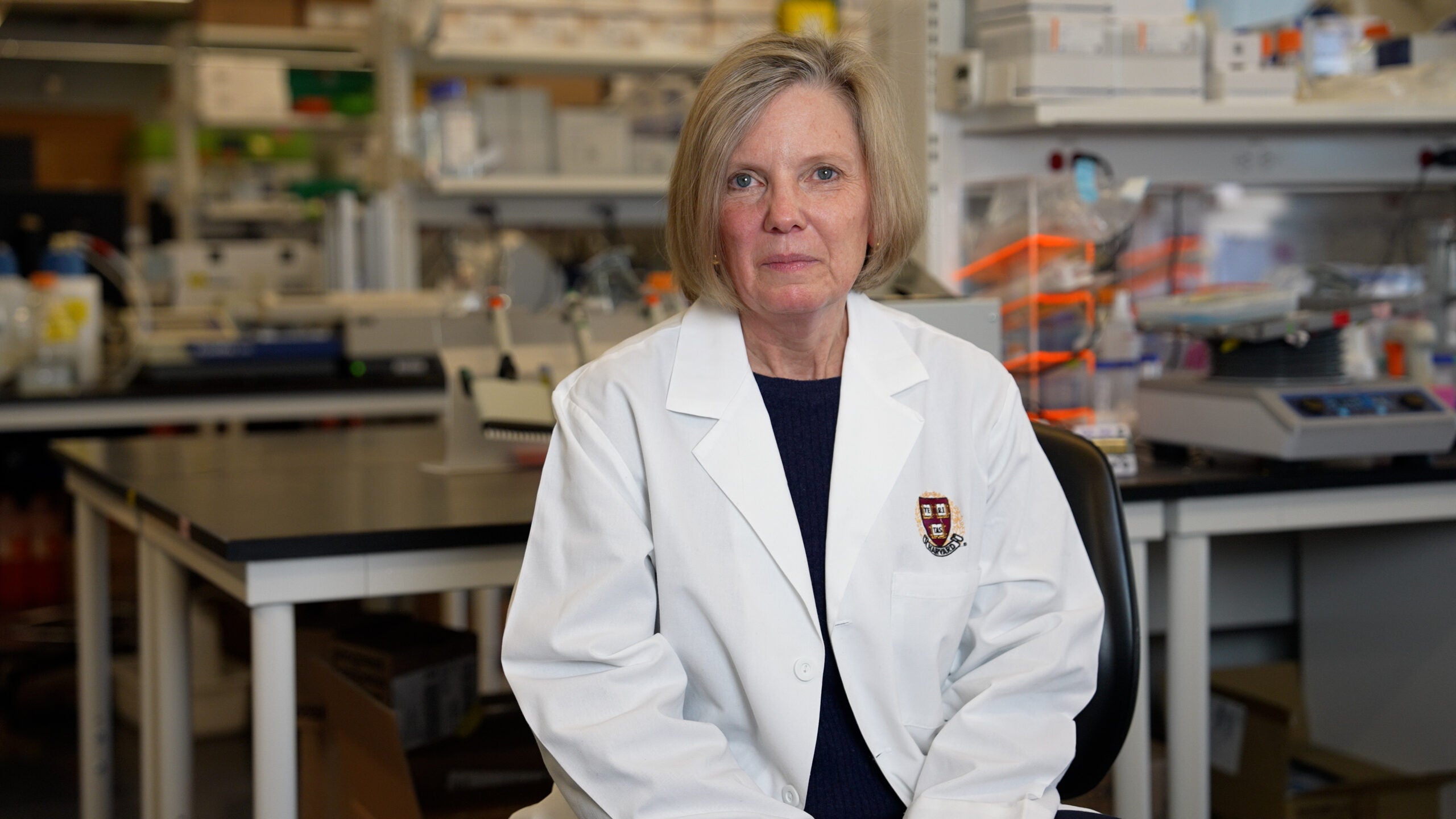
You’re listening to a press conference from the Harvard School of Public Health with Barry Bloom, professor of immunology and infectious diseases and former dean of the school, and William Hanage, associate professor of epidemiology and a faculty member in the Center for Communicable Disease Dynamics. This call was recorded at 12:00 p.m. Eastern Time on Wednesday, December 16th.
Transcript
MODERATOR: All right, Dr. Bloom, Dr. Hanage, do you have any opening remarks for us?
BARRY BLOOM: No, I think it’s very exciting to have two companies put forward new vaccines within 11 months and begin to roll them out to the public. That’s an extraordinary both scientific and logistical achievement.
BILL HANAGE: Yeah, I would echo that. I think it’s truly remarkable and it is a positive ray of light, shall we say, in a time when there hasn’t been so many of them.
MODERATOR: All right, first question.
Q: Hi, thank you for taking our questions and thank you, Nicole, for moderating. I wanted to ask you as a reporter, I’ve noticed that a lot of the articles that have done the best in the last few days have been about Bell’s palsy and anaphylaxis. I was hoping you could weigh in on the likelihood that someone getting a vaccine would experience a severe side effect like this, how it might compare to the probability of getting COVID-19. And if you could address, you know, obviously the FDA has moved more quickly on this than on other vaccines, but we know that most side effects from vaccines show up in the first two months. So if you just weigh in on some of the fears that the general public seems to have about the safety of the Moderna and Pfizer vaccines.
BARRY BLOOM: Thank you for the question. It’s been one of the favorites of the press. You know, in a trial of fifteen thousand people, to have two potential cases of a severe allergic reaction indicates this is not the commonest of vaccine reactions. My preference, by the way, is to distinguish between vaccine reactions, things that occur within a few hours of vaccination that occur with almost any vaccine and severe adverse effects or adverse effects that are scored up during the course of the trial. So with that, let me just start by saying virtually any vaccine that stimulates the immune response is going to produce a local reaction. Any vaccine that contains RNA and encapsulated lipids is very likely to stimulate an innovative response. And in some people, that will lead to an interferon response, which is a transient feeling like you have the flu, you feel lousy pain in the arm, fatigue, sometimes muscle pain. And what’s striking is every single possible adverse effect that you could think of is categorized and scored in both trials. Such that they come in two speeds. One is unsolicited. That is, they are just reported by vaccine volunteers and the others are soliciting their specific questions, are asked to be sure that we’re the vaccine companies are not unaware of anything bad that happens, and that means the data and safety monitoring boards are not at work. So with all of that, the number of adverse effects for vaccine reactions in my recollection of the Pfizer vaccine was about forty four percent and about eighty eight percent in the Moderna trial. I would also point out that Moderna has one hundred micrograms per dose of RNA, which is more than Pfizer has, which is 30 micrograms. So all I’m suggesting is that vaccine reactions are expected and probably indicate a good initial stimulation of an immune response. The two people who were reported in the AstraZeneca trial that had potentially severe anaphylactic reactions, which really could be quite serious, both had severe allergic states and both of them walked around with epinephrine containing pens, epi pens. But it was a good thing that we knew about it because it’s my understanding there will be precautions taken in the states for every vaccination place to be able to be prepared for any allergic reactions. The two ways to do that; one is, again, AstraZeneca did in one of their phase two trials, give an antihistamine before the injection, to head off allergic reactions or as the two people had their epinephrine present, where if there are signs of difficulty breathing, within minutes it can be injected. And these people both walked out, were not hospitalized and had nothing serious. So it’s a warning of a potential sign for a very small number of people. And I would think emphasizing the extraordinary safety in trials, now, they encompass thirty thousand and thirty-five thousand people that have had these vaccines is absolutely extraordinary.
Q: Thank you.
MODERATOR: OK, great. Next question.
Q: Hi, thank you. My question is for professor Hanage. I still remember that you are among the first one to explain the theory of herd immunity, and since now we have a vaccine on the way, when do you think that we can have herd immunity in the whole world and how can we talk about it now? And the second question is that also we know that many countries have promised to give the vaccine to the poor people and poor country. But there’s still a lot of challenges of vaccinating people in low- and middle-income countries. So how how can we face this challenge? Thank you.
BILL HANAGE: Thank you. Those are excellent questions. So to deal with the first, the notion of we’ve often heard about herd immunity, I prefer the term population immunity or community protection because herd immunity is an uncomfortable term in the first place, and it has become only more so over the course of the pandemic. But what it refers to is the fact that if a person is immune and unable to become infected or transmit the disease, then that immunity protects others because it means that they are unable to infect folks who would otherwise have been infected by them who are not immune. And we can estimate roughly what proportion of the population needs to be immune for this to be the case. Using some very, very basic mathematical models, you can make a much more complicated, but they tend to zero in on roughly the same kinds of sets of numbers, which is that given the mixing patterns we saw at the start of this and given the transmissibility of the virus, we would expect around 50 to 60 percent of people to need to be fully immune, maybe a little bit less, but to be fully immune, unable to be infected and unable to transmit the virus in order for what we call the critical vaccination threshold to be reached. And the critical vaccination threshold is the point at which a virus cannot invade a community. So with all that said, when you think about the vaccines we have at the moment, we are still a bit uncertain in the cases of many of them. We will hopefully get more information going forward, but we’re uncertain about the mRNA vaccines, about how able they are to prevent infection as opposed to development of severe disease, because it could be that individuals could be infected and still transmit, but not about illness. I suspect that that’s not happening a lot, but we still need to do some work in order to actually really nail that down. The best evidence for the AstraZeneca trial, that that does happen, meaning that people are unable to become infected and transmit. But again, that’s still stuff that we’re going to be finding out more about in the coming weeks and months. So having said that, that means a relatively large proportion of the population would need to be immunized with the vaccine in order to exclude the banks and exclude the virus from those populations. And that’s not going to happen overnight. As you alluded and despite the fact that we have extraordinary logistical challenges, but we’ve done extraordinary scientific work over the last year. When I say we, I mean humans in general, because it’s remarkable what the vaccine companies have done. We still have to actually vaccinate people. As I think Barry has said before, vaccinations don’t help any one vaccination does. And this is what you need to do in order to actually have the effect. And this requires the kinds of decisions that you’ve heard about. Who do you vaccinate first? Is it going to be somebody who’s going to be able to stop transmitting or is it going to be somebody who’s going to be vulnerable to infection? Many places are choosing to vaccinate older people of nursing home residents and health care workers first. And then you want to ensure equity in order to make sure that there is an equitable outcome in terms of vaccination within the population. And those are very important conversations to be had, decisions to be made. And finally, this is the last thing I’m going to say before I hand over to Barry, because I think he’ll have a lot more useful to say on this than I would. As you allude, there is a huge challenge with getting the vaccine to lower- and middle-income countries. Not only is that going to be a challenge in the first place, there’s also the fact that these mRNA vaccines need to be stored in very cold temperatures. And as a result of that, it’s unlikely that they’re going to be at least easily available for large parts of the world. And given the fact that it takes time to do this, it may really be some time before the entirety of the planet or very large numbers of people globally have received a vaccine. So we are on the way there, but we’re not there yet. And with that, I’ll pause and see what Barry has to add about rolling out vaccines of lower- and middle-income countries.
BARRY BLOOM: Terrific, Bill, thank you very much. We all hate the term herd immunity, and it’s a serious reason. It isn’t just because we’re not a cattle. Herd immunity provides protection for people who are not immune. That’s the whole point. So if you walk into a room with 80 percent of people who’ve been vaccinated and protected, you have a very low likelihood of being infected, but you’re fully susceptible. And that’s what we mean by herd immunity. The immunization of a percentage of the public protects, to some extent, those people who are not immune. Any one of those people could walk into a room with someone with COVID and 80 percent of people would be protected, but that person would get COVID. So that’s the objection. And I think community protection is a favorite term by all the scientific community except for the press. On this subject, there was a paper that came out a week ago that got some coverage in the press, which looked at what percentage of the people were seropositive, had antibodies to COVID in the city of Manaus in Brazil. And that number was something like 65 percent. And the newspapers in Brazil and the coverage here raised the question, does that mean herd immunity has been achieved in Brazil if eighty six percent of people are seropositive? And this is somewhat of a technical concern, but I think it’s sufficiently important because it would prevent drawing that inference. You measure two possible things in a serologic test. The most abundant antigen in the virus is the nucleocapsid protein, so most antibodies are directed at the N protein, and the N protein does not protect against infection. So you can have whopping amounts of antibodies to the N protein and have zero level of protection against infection. It appears that to get protection, which is why the spike protein was used to make the RNA in the first place, is you need antibodies to the spike protein to get protection. So what has to be very careful about percentage zero positivity, the most commonly used assay is measuring whether you’ve been exposed to the virus by antibodies to the N protein, tells you absolutely nothing about whether that individual is protected or not. How do I know that the antibodies to the protein are required for protection? In a sense, I believe the evidence is forthcoming that it correlates extremely well with protection, but most strikingly, a recent study has been done by our colleague at Beth Israel Deaconess, Dan Barouch, in primates, where they took convalescent serum from people with anti-spike proteins and they showed they could protect monkeys. So by itself, antibodies to the spike protein are sufficient to protect primates. We assume the same is true for humans. And the one critical study showing that is a crazy study, but I think wonderful, of a fishing boat with one hundred and twenty people from Seattle, that went out. Everybody was tested and had blood taken before they left. Everybody was COVID negative when they left. 18 days later, one crew member got quite sick with COVID. They returned to shore and when they returned, something like one hundred and eighteen members of the crew became COVID positive from one patient where they all started COVID negative. The only three people who didn’t get COVID, were people who had antibodies before they left, which was only ascertained after they came back, and they were antibodies to the S protein. And that was pretty definitive evidence for me, that if you have antibodies to the S protein, if they have a high enough level when they last long enough, you’ll get protection. So along with an answer to the question, be careful of how to interpret serologic epidemiology.
On the subject of the wonderful question on developing countries, as I understand, it’s a vexed question and it shouldn’t be. So, as you know, the US has pulled out of the World Health Organization and will spend no money, spending money on this consortium of donors created by the Welcome Trust, by the Coalition on Epidemiological Preparedness and Innovation called CEPI, that has underwritten many of the vaccines being tested. A number of other countries have put in some funding or are committed to putting in funding. One hundred and eighty-eight countries have agreed to be part of that and have some fair process for distributing funds for purchase of vaccines and distribution of vaccines around the world. As of a recent report, I am really sad to say two things are happening. One is the money is not coming in. COVAX, the name of the consortium, needs two billion dollars and they have a tiny amount of money right now. A couple of hundred million dollars maybe in promises. Number two, middle income countries are bailing out of COVAX and trying to negotiate favorable terms for their countries, which means it is every man, woman, child and middle-income country for themselves. And equity will go out the door. That’s extremely worrisome. And then finally, the rich countries are in this context, buying up commitments for all the vaccines they possibly can. So Canada has now formal commitments for five times more vaccines for multiple providers than the entire population of Canada and is beginning to think about what to do with the extra vaccines that they will end up having been committed to. We are buying additional commitments for vaccines, as you know. So I guess my sense is we’re at a critical point for the middle, low and middle income countries in that, all the money for vaccines is committed to the existing companies to go to the rich and a small number of middle income countries, there’s not going to be any vaccines for anybody else. And that’s a morally unacceptable condition and scientifically unacceptable, because not only will people die there, but they will travel around the world and bring the vaccine back to all of those who have chosen not to get it. So we’re at a pivotal time and I don’t usually lobby the press, but with a new administration coming in without the US as part of that, I’m fearful that the COVAX Equity Initiative can distribute funds for vaccines around the world will fail.
Q: Thank you. Thank you so much.
MODERATOR: I’ve got a couple of links in the Zoom chat to some of the papers that Dr. Bloom was referring to. Next question.
Q: Yes, hi, and boy, what an eloquent response that was to the international scene. So anyway, I hate to pivot you back to a science question. Can you elaborate a little bit on the innate interfering response, like what’s science or the medicine behind when we do get vaccine reactions? What’s going on? And is there a simple explanation for why one vaccine, the Moderna vaccine, might have a slightly higher vaccine reaction than Pfizer? And then finally, just when people do have an allergic reaction, what are they reacting to?
BARRY BLOOM: Yeah, great. All great questions. So let me start with vaccinology, about 1910. Most things that we want protection against are proteins, sometimes carbohydrates for bacteria, but mostly proteins on the surface of, let’s say, viruses. They’re important for binding to receptors, they’re important for entering cells, and if you block that, you tend to get reduced infection or protection. So you take almost any protein and put it in saving and stick it in somebody’s arm. You either get no immune response or really pitiful immune response. So most proteins do not stimulate enough of an acute reaction to a foreign protein to show up. So in 1912, people decided to put the proteins on aluminum, aluminum hydroxide. And for almost one hundred years, that was the only adjuvant, an adjuvant is something that is designed to enhance the immune response to a real antigen, that was why your tetanus shot hurt. And it hurt because the alumina was a foreign body. It triggered an innate immune response. Many cytokines are released, among them interferon, beta, probably tumor necrosis factor, TNF. But these are things that cause inflammation. Inflammation brings macrophages, dendritic cells and white cells to the site and enables very efficient uptake by the cells who can carry antigens to the lymph nodes and spleen to generate a good immune response. So when we say that for reaction at the site of injection is a good thing, it really is. It’s reflecting an immediate response to a foreign material that will ultimately enhance the immune response to what you wanted to enhance. Now, you ask the question, what are the components of vaccines that trigger that? Well, in the case of tetanus toxoid, it’s aluminum hydroxide and it’s put there precisely to do what we’ve described. In the current vaccines, there are two components, and I don’t think anyone knows which of those contributes most to the vaccine reaction. One is complex lipids that are used to protect the RNA, which is easily degradable, and deliver it through cell membranes to get it into cells, to become able to be processed and presented to white cells to produce antibodies. So, the lipids could well be a part of the toxicity. There is no lipid alone control in the placebo group, so we have nothing to compare lipid by itself with in these trials.
The second point is, one of my favorite situations is when people were trying to use RNA for preventing cancer, correcting genetic defects, one of the real problems was RNA from viruses. Every cell has RNA. But RNA from viruses was really quite toxic and really would have mitigated the use of RNA therapy or vaccines or anything. And there was a woman named Katalin Karokó who was at the University of Pennsylvania. And when everybody gave up on therapeutic use of RNA, everybody, they thought she was a nutcase. They couldn’t get her brains. She had a wonderful boss who has protected her and provided her with a position at Penn. And she worked out a way to eliminate the acute toxicity caused by RNA, by changing one of the four bases that are the building blocks into a modified base that generally doesn’t occur in nature. That’s the breakthrough that is allowed people to stick RNA into people without really serious adverse effects. Having said that, RNA still has toxicity. And I would point out that the Pfizer vaccines have 30 micrograms per dose, the Moderna vaccine has one hundred micrograms per dose, and my reading is that while none of them had serious adverse effects or vaccine reactions that you worry about, the percentage of people reporting complaints, sore arm fatigue, muscle pain was a bit higher in the Moderna vaccine. And that may be because the lipids are different or because there’s more RNA. A long-winded explanation, but I think the bottom line is local inflammation helps disperse the antigen into the places in the body that are needed to generate an immune response effectively.
Q: Thank you. And then when people do have these very, very rare adverse allergic responses, then are they responding to the lipids, do we think?
BARRY BLOOM: Unclear.
Q: OK.
BARRY BLOOM: In the case of these two vaccines and even in the case of the adenovirus in the Oxford study, totally unclear what component these two individuals were allergic to. And let me just distinguish between people that have severe allergies, from a vaccine reaction, which is a normal innate immune response to a foreign irritant. These people had really serious allergies and walked around with epinephrine pens. So whether it was food allergies and some of the components in the vaccine might have had some component of serum that cells were grown in or some protein from the cells that they were cultured. And so we really don’t know what triggered their allergic responses. Again, I would point out thirty thousand people, at least 15 to 20 thousand people have had that vaccine and only two have reported severe acute allergic reactions.
Q: Perfect, thank you.
MODERATOR: Next question.
Q: Hi, thanks so much for doing this. I just wanted a little bit more, if you could wax poetic again about the impact of having a second vaccine and what that will do for the country, and will it create confusion or is it all good?
BARRY BLOOM: I will turn that over to my friend, Dr. Hanage.
BILL HANAGE: That was a really good explanation about allergies. But I was going to just add at the end, because I was thinking about it, the great example of allergy and a vaccine would be influenza vaccines, which have often been grown in hens’ eggs. And so if a person has an allergy to eggs, they are not, you know, this is one of the reasons why if you have a flu vaccine, people ask you whether or not you have an allergy to eggs. But moving on to wax lyrical about this, it’s quite remarkable the fact that we have not one but two MRNA vaccines now at the end of 2020, when at the start of 2020, we don’t have any MRNA vaccines. And as we were just hearing, there was a lot of concern, you know, there had been historical concerns over whether or not RNA was something which could be used in this fashion. Now we have two of them. They have similar efficacies, not identical, but quite similar. It appears to be the case. And the nice thing about the Moderna vaccine is that it is able to be transported and stored at somewhat higher temperatures, minus 20, as opposed to minus 17. And minus 20 freezers are much more common than minus 17 freezers. And so this may mean that there’s going to be a much greater opportunity to be able to get the vaccine out to a larger number of people more quickly. The actual rollout of vaccines, we are going to likely have multiple available and we already have multiple available. And as a result of that, that can only help us. I want to add one other thing to what Barry was saying earlier about the truly depressing emergence of what some people call vaccine nationalism. One of the things that this year has made abundantly clear to me and other people who work on infectious disease is how little a lot of people get the idea that of what infection means. It means an infectious disease is transmissible. An infectious disease elsewhere in the world can infect people here, provided there is still movement of people or you can infect people who are not vaccinated, are not protected anywhere. And so it is very, very depressing to hear any kind of approach to public health that does not prioritize stopping the virus everywhere. And not only in one place. We are all human beings, and we all deserve protection. And having said that, I will let Barry say anything he wants to add about Moderna.
BARRY BLOOM: I think having two vaccines is terrific, and as Bill said, with the minus 80 vaccine, it really comes in nine hundred and seventy-four vials per box that has to be kept at minus 80. So it’s really terrific for distribution through hospitals, where you can line up a whole lot of people and use the vaccine efficiently and not have it go to pop. There are community centers that have freezers where obviously it can be distributed locally. The advantage of the Moderna vaccine is twofold. It would really be a lot more practical for rural areas because you don’t need to carry on with dry ice and you don’t need nine hundred ninety-four people in your local post office to line up to get one box worth of vaccines. So I see them, as Bill said, of really comparable effectiveness and safety and rather complementary epidemiological value of where they can go and go quickly.
BILL HANAGE: Yeah, I completely agree. There’s only one caveat that I think is important for people to get here at this point, which is that it can take a lot of time to vaccinate a lot of people, a lot of personnel and if you look at the I think in the 2010 census, there were something like one hundred million people in the United States over the age of 65. And so when you’re looking at vaccinating that many million people, it’s not going to happen overnight. This is why we have to have priorities that we’ve been discussing previously and the fact that we have two vaccines, one which is able to be used in major health care centers, as we were just hearing, and another which is more suitable for use in the post office, is going to be a real help. On the other hand, you know, it’s still going to be a major logistical effort to get a large proportion of Americans vaccinated.
MODERATOR: Do you have a follow up question?
Q: Yes, thanks. This morning at a press conference, Secretary Azar said, I believe three times, that Pfizer was having production issues. Do you know anything about that? And if not, knowing the process of creating these mRNA’s, do you have any idea what the difficulties might be, what might be hard about making them at scale?
BARRY BLOOM: I don’t know the answer. They’ve had production problems before, and that’s why their initial promise of one hundred million doses by the end of the year was cut back to 50 million doses. If you want to have a sense of the complexity of getting these vaccines from a company to people, the first place to start is to walk through, get a visit to a major vaccine production company. It is the most complicated Rube Goldberg place that I’ve ever been with tubes and tubing and electronic stuff and whatever. There are a million things that can go wrong, not least getting needed supplies to have the whole thing operating and running that may be no fault of the producer itself, but it’s very complicated to scale up. An example, for the chicken pox vaccine, the varicella vaccine. It worked on a small scale for MERS within years. They made the vaccine. They were simply unable for another 12 years or so to scale it up to a level that they could guarantee safety and effectiveness at an economic scale where they didn’t have to throw out more batches than they were producing. So it’s one of the more complicated production things imaginable. You see on the newsreel, all these little vials going around, and I think one computer glitch in the whole place shuts down. I am astonished, to put it this way, I don’t know how many of these production facilities are new or how many of them are old facilities that have been reconverted, but in general, if you want to make a new vaccine, you have to build a new building and buy everything new. That cannot have been done here because they couldn’t have done it within a year. So some of these must be repurposing existing facilities as well as extending new so-called lines of production where you just have parallel lines of doing the same thing four times over within the same or a different building. It’s complicated. So one shouldn’t be surprised. And I don’t think the companies can be criticized for not meeting the timescale.
MODERATOR: Next question.
Q: Yes, hello, gentlemen, thank you very much for taking some time to talk to us. Boston has one of the highest proportions of health care workers in the country. I think we rank third for how many the proportion of our population that works in health care. That would seem to suggest that a lot of people, a greater proportion of our population is right now getting vaccinated or will get vaccinated in this first wave. Is that likely to have any sort of effect on the pandemic locally? Will our drop off curve be quicker in Boston because we have more health care workers?
BARRY BLOOM: That’s an interesting question. You could ask another set of questions, whether that’s fair or not. I don’t think it’s going to have the major impact, other than the fact that we have very good health care in Boston, and we have a fair number of beds that are occupied now. And so I sat on the governor’s commission for allocation of vaccines with a larger number of people. I’ve sat on a lot of committees in my life, most a total waste of time, at least in academic institutions. This was an absolutely inspiring experience. We had members of black and Hispanic communities. We had the mayor of a town with a high burden. We had religious leaders within the community. We had someone from Children’s Hospital, chairman of medicine in a major medical center outside of Boston. And given the task of where do you assign something in really short supply, in desperate need? The first thing I wanted to say, and I would think would be a great story in any city in this country where serious people were brought together to deal with who gets and who doesn’t get in when, there was a level of citizenship and moral reasoning that we all know the answers can’t be perfect. But the decision here is to take medical personnel that are face to face with patients that have COVID in the hospital. Those are the people that have the greatest risk. If you work in orthopedics in another part of the hospital and don’t see COVID patients, you will not be first in line in Boston in the early days to get the vaccine to come out. But if you’re in environmental services, if you are one who is a nurse that is working with the patients or someone cleaning up when patients die and have direct contact, there was no question that these people are as exposed as the fanciest and most important doctor and chair of an ICU. And unanimously, everybody was keen to bring them into the first category. So I don’t think every doctor is going to get it before every incarcerated prisoner in Massachusetts. I think the efforts were made to distribute it with every consideration for vulnerabilities, for risk and for equity to be honest.
BILL HANAGE: Yeah, I was not on that, but it’s an extremely inspiring thing to hear about. I can only thank everybody involved. In response to the question, I would estimate at the moment, roughly speaking, that maybe 13, 14 percent of Massachusetts has actually already been exposed to the virus or at least had some infections. And as you know, cases are continuing to tick up here and continuing. So that shows how far away we all from any population immunity. I think that while I’m delighted that, as you say, patient facing health care workers, I was just saying those are the people who really need it. I’m glad that they’re receiving the vaccine first or among the first because of the fact that these people are at risk of infection. There was a study that was done back after the spring surge in a London hospital, which found that as many as, I think it was over 40 percent of patients facing staff had evidence of infection. So these people are really high risk and it’s right they should receive vaccine. However, I don’t think that the numbers of them are going to be large enough to make a very major impact in the Boston area on the course of the pandemic. I think that we are going to be happy that they are going to be protected, but it’s not going to be a large enough proportion of the community to make a very noticeable difference.
BARRY BLOOM: You know, that raises an interesting point. Again, I was impressed not only with our committee, but with the government representatives in the public health department and from other parts of the state government. We know how many people in the state of Massachusetts are in every single priority category. So when Bill said this is not going to make a major difference in the epidemic, there are one hundred and sixty five thousand people in the clinical and non-clinical health care workers doing direct work on COVID patients. That the state could pull that together in like two weeks’ time at every level in every district, and every state has been asked to do the same, to give their priorities for what they would do with the vaccines when CDC approves it. Not every state has done the kind of work done here, but one hundred sixty-five thousand people is not going to change the epidemic in Massachusetts. It is going to protect the hospitals.
MODERATOR: All right, next question.
Q: Hey, thanks for doing this. You mentioned a bit about how they’re still studying whether a vaccinated person can transmit the virus. Just to kind of bring a home for people with a real life example, if my neighbor is a doctor and he’s been vaccinated and I still have not been vaccinated. What should people know about that? Should he wear a mask when he interacts with me? Should I wear a mask when I interact with him? Should we both be wearing masks still? Could you just kind of address that kind of situation?
BARRY BLOOM: I think it’s a great question, and I think you have exactly the right answer. One of the worries that I think we all have is that once people are vaccinated, they will assume they can’t be infected again. We’re grateful for the fact that very few re-infections that have been demonstrated to be re-infections have occurred in people with prior infection. But I would point out with the ninety five percent protection, which is spectacular, still five people got COVID that were vaccinated and 90 people who weren’t vaccinated got COVID. So the public health answer to your question is your answer. Until we really are confident and know enough about whether if you’re vaccinated, A, you really are protected against infection and for how long, and B, if you won’t get sick, are you able to shed virus? Everybody has to keep wearing masks, socially distancing and taking public health precautions. And that’s going to be hard to keep the morale up to do that, because everybody thinks when they have a sore arm, they’re protected forever. And we don’t know that yet.
BILL HANAGE: It’s an absolutely super, super important point, and for the reasons that Barry said, and also because there is just the point of morale, which is that we want people to continue to be wearing masks. Yes. And if some people are not wearing masks and it becomes sort of acceptable for people to say, oh, no, no, I’ve been vaccinated. Well, we don’t know that necessarily. If you see someone in the grocery store not wearing a mask. So given the fact that we do not know yet exactly how the force of infection will vary with the numbers of people who have been vaccinated, it is of the utmost importance that people continue to use masks and social distance as we go forward. Now, the other reason for that is that we don’t actually know until we have a large amount of population vaccination what the virus will do in terms of evolution or selection, because that’s only then that we’re going to be able to determine what actually happens at that point, because there won’t be enough selective pressure on it until that point. So we’re going to need to continue to do these other measures, and then, like I was saying, to closely monitor what is going on in the population, both in terms of testing, perhaps in terms of wastewater monitoring, in order to see how much is being shed and relate that to the numbers of people who are being vaccinated. And once we are confident that it is under control and that once we have got more data on whether or not individuals who have been vaccinated are able to become infected and transmit, then we can revisit these things, then we can do that. But right now, everybody is being vaccinated. I would still say wear a mask.
Q: Yes, thank you.
MODERATOR: All right, next question.
Q: I would like to follow up on the issue of morality and access to vaccine in low-income countries. So I have the impression that the Western countries are kind of the hostage of a big pharmaceutical companies. And I’m wondering why there is no action in the US on the monopoly of licensing rights, which actually would allow for a third party to be selling licenses and increased production of vaccines while decreasing the price, making it much easier for Western countries to buy vaccines also for developing countries. So I would like to have your opinion on that.
BARRY BLOOM: Yeah, it’s a very good question. So there are two parts to the question. The first is some licensing and licensing of the existing technologies are already underway. The specific best case right now is the Serum Institute of India in Pune, India, that makes more vaccines of high quality than any other vaccine producer in the world. Many of the vaccines used all over the world are produced in India and then what’s called the Fill-in finish are sent in bulk to named companies that then put them in bottles, label them and distribute them. So the Serum Institute was given a license by AstraZeneca to produce their adenovirus vaccine and they made a commitment to provide half of it for India and used another half of it to distribute through COVAX or elsewhere to low and middle income countries. A number of middle-income countries are increasingly trying to cut licensing deals. The limiting factor is there are very few middle-income countries that have the technical capability to produce vaccines of quality of high scale. For example, I was surprised to learn recently I gave a talk to University of Cape Town in South Africa. There is no vaccine producer in South Africa. They can take vaccines and finish and fill and put them in a bottle with a label on it. But they don’t have the ability right now to produce the vaccines. Other countries have licensed stuff from China to be able to produce the wholesale vaccines from China, Indonesia and Malaysia are able to do the same. So that’s part of the question.
The other is a more complicated question that I don’t think we have yet to face is the issue of licensure, and that is, are the prices going to be so high once the vaccines are approved and able to be sold and not just provided by governments? Low- and middle-income countries won’t be able to afford them, and I would only say that several vaccine producers, including Johnson and Johnson and AstraZeneca, are talking about their vaccines being priced on the order of three dollars to five dollars apiece. If that’s the case, there’s not a lot of patent issues. And in the States have agreed to do the same to produce at minimal profit until there’s a significant amount of vaccine provided. So I am hopeful if Canada can get five times the total population by the end of summer, we may have an excess of vaccines for the rich countries and they will still be committed to paying for them. They might claim to distribute them in some rational way through the WHO to developing countries. As the year progresses, we should have enough for the whole world by the end of 2021. Who will pay and how it will get distributed is unclear? But if they were paid, at least they would be available for distribution.
MODERATOR: Are you all set?
Q: Yes, thank you.
MODERATOR: Next question.
Q: Thanks so much. I’m curious, even though the two vaccines, Pfizer and Moderna, are created off the same platform, there are some differences. And I’m wondering if you can address some of the differences between the two vaccines that the average person might be interested in. For example, why is Pfizer saying take the second shot at twenty-one days and Moderna saying take the other shot at twenty-eight days? Why the difference in the temperature that they need to be stored in? And Dr. Bloom, you mentioned that Pfizer uses thirty milligrams of RNA per dose versus Moderna is one hundred milligrams. If you could chat a little bit about the differences between these two products.
BARRY BLOOM: So thank you for the question. It’s certainly a wonderful question. Let me just correct you. It’s 30 micrograms and one hundred micrograms. A million per gram, not a thousandth of a gram.
Q: Oh, sorry. Thank you.
BARRY BLOOM: Just to clarify. Immunology, I would like to believe, is a science. Epidemiology, I have my doubts, but Bill has just persuaded me it, too is a science. Producing vaccines is absolute alchemy. And what I mean by that is that there’s an awful lot of rational thought that goes in. And then there’s an awful lot of empiricism. So all of these vaccines before they got into humans may even start before they, which is one of my favorite subjects. The platforms for these vaccines were made long before COVID existed. So the RNA platforms were developed for influenza. Moderna had two strains of influenza. They had a MERS vaccine. I can’t remember the names, but I think Pfizer has a respiratory syncytial RNA vaccine. These platforms were developed to create vaccines quickly for any new pathogen, and they were all tested in animals before COVID happened. They worked out the doses, the toxicities, the amount of time between the primary and the booster shot in animal models for other vaccines. And when this hit, they went empirically in the animal studies for COVID, which did precede any of the Phase one trials in humans. To find out what times dosage seems to work best and its trial and error, and you do three doses, even in the phase one studies, each of these did three different doses to find out which one gave the best immune response with the least toxicity. And they did lots of experiments in animals to find out for their combination. The principal difference is not so much in the RNA, it’s in the lipid droplets that have adjuvants associated with them. They’re very complex and quite different. And they would have different requirements, different temperature stability. And my guess is over time, Pfizer will play with some alchemy, change the lipids and try to produce it. That works at a higher temperature for storage. And it may even be that Moderna works to have the minus 20 go up to plus 4, which you can do for adenovirus vaccines. In any rate, it’s empirical trial and error, a different kind of science, but equally difficult. And I admire it immensely.
Q: So the 21 days versus the twenty eight days is not a significant difference?
BARRY BLOOM: I don’t know the reason why that turned out to be different. I think they’re two just on basic principles. So let me start with the first vaccine that was ever put into humans for COVID, which is a Chinese vaccine that put the spike protein of Coronavirus-19 into an adenovirus platform. And the one that they used is a very common adenovirus called adeno-type-five. But my reading of the data is they got a poorer response than either the people in AstraZeneca or J&J, and the reason is about 30 to 40 percent of Westerner’s and 60 to 80 percent of African populations have already been exposed to adeno-five. So when you put the adeno-five virus recombinant into a person with antibodies, they simply clear the antigen. And it’s less immunogenic. And the Chinese vaccine is not nearly as good a vaccine as picking a chimpanzee adeno that humans have no prior exposure to or adeno-twenty-six, which is a very rare strain. So one of the timings is you want to boost at the latest possible time. So that you can avoid antibodies produced to the priming experiment that will tie up and clear your booster shot. On the other hand, for practical purposes, you have to get that in before those antibodies are high enough to tie up your vaccine and hence, you’re working with a narrow window enabled to do that. So the priming will produce antibodies. In both trials, the people made antibodies you could tell just from the curves, by 14 days they were already getting some immunity. If you wait much longer, when the antibodies level come up, the boosters don’t boost. That’s the bottom line from the time.
MODERATOR: I’m going to break in here really quickly, Dr. Bloom, it’s 1:03. Do you need to run off to another meeting or do you have a few more minutes?
BARRY BLOOM: I certainly have a few more minutes.
MODERATOR: OK. Dr. Hanage, do you need to go?
BILL HANAGE: I should probably go in a little while. I was going to add to Barry’s point. I mean, he knows much, much more about vaccines than I do, but I was just going to observe that it’s far from uncommon for people to take licensed vaccines and tweak with their schedules and figure out what best way or the most effective ways to deliver them and achieve a good immune response. So this is something that is expected to continue to happen and perhaps be tweaked for quite some period of time.
Q: Are there any other differences between the two that people should be aware of?
BILL HANAGE: Not that I’m aware of.
Q: Thank you.
MODERATOR: Next question.
Q: All right. Thanks for taking my question. I just wanted to get your thoughts on people who have already had COVID, whether they should be vaccinated, and what’s the prior prioritization on that? There have been various ideas floating about whether those people should wait longer, for example.
BARRY BLOOM: So I think the guidelines for providing vaccines when you’re dealing with fifteen thousand people in trials, it was simply not possible to test every one of the volunteers before they entered the trial. Thirty thousand tests to find out who had already been exposed to COVID. So one of the good things about not doing that, since there were no serious adverse effects that seem to be related as to whether people had had exposure to COVID in the trials, it suggests that vaccinating someone who has had exposure, who may or may not be protected, as I mentioned, they may or may not have antibodies to this protein, hopefully they do, but there seems to be no harm in vaccinating those people. And it hasn’t produced any of the concerns that have occurred in other vaccines for enhancing the exposure to virus and making them sick. So those are things that just fell out of the trial. And I think people are being asked if they had exposure to wait a period of time before they take a new vaccine, if they’re in the right age and priority class.
Q: OK, thank you.
MODERATOR: Next question.
Q: Hi there. Can you guys hear me?
BARRY BLOOM: Yes.
Q: OK, great. Thank you so much for taking the question. I have a couple following up with some of the things that you guys have said. This was covered in the past, but I’d like one of you maybe to refresh our memory. This particular vaccine, does it give you COVID or gives you protection from this virus, being that flu gives you somewhat of a flu. So in very basic terms, does this vaccine give you COVID? I would like to reiterate for our viewers and listeners what it is.
BARRY BLOOM: Absolutely fundamental question. There are very few things that in my world I can say with certainty. This is one of them. There is no virus in the vaccine. There is no replicating ability to multiply and produce the virus. So you cannot get COVID from this vaccine.
Q: Thank you very much, going back to the question of, I hate to trigger you guys, herd immunity, so just ignore that I said herd. Is there a magic number, let’s say, in the US like we know the population? Is there a magic number of the people who need to be immunized that we are aiming for in order to turn the page on COVID in this country?
BARRY BLOOM: Bill?
BILL HANAGE: So the number that you’re thinking about there is usually calculated as the critical vaccination threshold. And for a vaccine, which is one hundred percent effective at preventing infection and transmission, some very simple high school math, which I’d go through if that was a blackboard here full out, that number is 1-1/R0. Now, R0, for this, which is the number of people who are infected if you were to drop an infected case into the middle of a completely susceptible population, the average number of onward infections that would happen from that is estimated to be between three and four, around that may be a little bit lower. And that depends on the contacts patterns that people are making. It does depend how much people moving about and how much they’re making contact with each other, which is why it’s not a sort of universal constant. So if that’s the case, then we would expect around 60 percent of the population to need to be vaccinated. In reality, of course, some of the population, as we were just hearing, will have already gained some immunity through being exposed and infected. It’s also true the population contacts and the way in which we contact each other means that the actual number is probably somewhat lower than that naive estimate, because that estimate is kind of assuming that we move about like molecules in a gas randomly contacting each other. But in reality, of course, we’re much more likely to have contacts with, for instance, people in our own age group. And as a result of that, the number is probably somewhat less. So there is not a number that scientists are aiming at, but for the public to understand the point at which it is going to be having a really significant effect upon transmission. I think that probably 50 percent or so, 40 to 50 percent is the kind of number that you would want to be. That would be helpful to think about that. And that thinking, which is why my answer previously about, for instance, number of health care workers in Massachusetts and what the impact of vaccinating them might be. That was why my conclusion was that though it’ll be important and it’s good that it’s happening, we don’t expect it necessarily to have a huge impact upon population transmission rates.
Q: Thank you. And the last question for me, I know we have to wrap up. A number of states are getting ready to vaccinate the elderly. So the long term facilities, either next week or the week after. Again, it has been covered, but refresh your memory. What, if any, side effects could folks who are older, experienced and need to watch out for? Is it obviously safe for them? And then the last thing is, do we have a timing for child vaccinations?
BARRY BLOOM: So every one of these vaccines is being tested in people over the age of 65. Something like eighty percent of deaths or more have occurred in people over 65. So it is the vulnerable population in nursing homes and assisted living facilities. Many of the people are very fragile. But what was striking in the trials is the vaccine reactions were lower in the over age 55 group than it was in the younger group. So I would expect fewer problems with the initial vaccination. But these are frail people in many cases, and there may be unknown consequences of stressing them with even as little thing as a vaccine. But there is no the bottom line is the vaccines have been tested in the elderly populations. They’ve been tested in people with a wide variety of comorbidities, single comorbidities, and there is no safety signal that has come up different from those among younger, healthy people. So I would not expect a great deal of difficulty. The other point I would make is, you know, that older people respond really poorly to many vaccines for the flu vaccine. They don’t do very well for shingles vaccine. Initially, they did very poorly and then they changed the vaccine in at an adjuvant, and it’s now even in elderly people on the level of over 90 percent. So the hope is that these vaccines have produced over eighty-seven, eighty-eight percent protection in the over 65 group, which means that they’re able to respond remarkably well, maybe only slightly less than younger people to both vaccines. That’s very reassuring.
Q: What about the vaccines for children? That was my last question.
BARRY BLOOM: Children have not been included in the vaccine. I think the reasons are obvious. Children can’t give informed consent to take anything until it’s become proven to be safe and effective. And children in this circumstance turn out to be infectable and able to transmit but get much less sick and seem to transmit less well than adults. So until the vaccine is proven to be safe and effective in older groups, they will not be putting this vaccine into children. Pediatricians I know are unhappy about that. But I think from an ethical point of view, you don’t put stuff into people who can’t give their informed consent with something you don’t even know how safe and effective it is. Once it is licensed, even with an EUA, emergency use, children’s vaccine studies will begin, pregnancy and lactation trials will begin. These will not be necessarily randomized controlled trials. These will be safety trials to show that there is or is not a benefit and that the vaccines are still able to work on a smaller number of people do not produce any adverse effects.
BILL HANAGE: With that, I’m going to have to leave. Barry, it’s great to see you, I’ll have to check in with you before the holidays, but if not, I’m sure I will at some point. But great to see you, great to see you all. Take care of yourselves.
BARRY BLOOM: You too. OK. I can stay for another 10 minutes.
Q: Nicole, thank you so much and professor, thank you so much for your expertise and time always.
BARRY BLOOM: Anybody else have a question?
Q: Hi, thank you so much for staying after the allotted time just to answer our questions. Mine is in regard to people taking the vaccine. So some polls have suggested that, yes, while people are willing to take the vaccine, a lot of them actually just want to wait before taking it, whether it’s to see if more data comes out or to see their neighbors take it and see what the outcomes are. So what would be sort of your answer to that? Like, why should people be taking the vaccine now instead of wait?
BARRY BLOOM: If people had read the fifty-three pages of the FDA evaluation of the Pfizer vaccine and the fifty-four pages of the FDA independent advisory committee of the Moderna vaccine and looked at all the data, I think they would all be very confident tomorrow to take the vaccine. So the real issue isn’t whether there is evidence that these vaccines are safe and effective, at least for the time period that things are under way. And we’re in the context of that, the virus is out of control. So your chance of getting sick or dying is a lot greater going to the grocery store than going to get a vaccine. I guess my feeling is it is appropriate in this not to be shamed if people are skeptical or have doubts about how safe and effective these vaccines are because they haven’t read the one hundred seven pages that I’ve read. And a lot of the people providing the vaccines have read and they need to see that they really are in real life, safe and effective. So I think asking the question is right. I think our job as scientists is to provide the information that we have, and I think the providers have as well. The companies have put out forms that tell everybody who volunteers for a vaccine now to give them a rundown of all the anticipated vaccine reactions that they could expect to have, and all that people are being very forthcoming. But the real answer will come when people within their realm of community take the vaccine and advocate for it and say it wasn’t so bad. And I feel a lot better knowing that I can go outside, and I can go to work and I think I’m well protected. This will be a slow process. There’s no magic pill or bullet for changing people’s behavior or inspiring confidence. I think it will have a fair number of skeptics at the beginning. I think as we see more and more people taking things perhaps halfway through the spring beginning to open up, more people will want it. And what will really make the difference is when more people want it, then there is vaccine, when there are shortages. That’s when the demand will really peak. And we’ve had an experience with that vaccine company shut down and we have about 50 percent coverage for influenza vaccines when the year the company was shut down for production problems, the demand for vaccine, certainly in Massachusetts, shot up people who never got vaccinated before once they heard there was a shortage, were first in line for vaccine. So I’m confident that the early vaccine recipients don’t have big problems and they begin to see things, numbers going down, the curve going down. I think there’ll be an increasing demand except for a very small number of people who will be anti-vacciners, and they will be the people who will be protected by herd immunity. They will be the beneficiaries.
Q: Thank you.
MODERATOR: And it looks like this is our last question.
Q: Can you hear me?
BARRY BLOOM: Yeah.
Q: OK, thanks for speaking a few different follow up questions, questions that have already been asked.
BARRY BLOOM: Would you speak a little louder, please?
Q: Yes. Can you hear me?
BARRY BLOOM: Yes, very well.
Q: Sorry about that. I’m curious. You talked about the vaccines and effective with the elderly population. Will certainly vaccines give more protection to certain populations like the elderly, like to certain ethnic groups, like to people with certain preexisting conditions? That’s my first question.
BARRY BLOOM: Great question. I wish I knew the answer. I can tell you what I wish for, I wish, like measles vaccine, it would protect one hundred percent or ninety-five percent of everybody at every age group, every ethnic group. We haven’t seen any vaccine that I’m aware of, huge differences in immune responses by ethnicity. We’ve seen elderly people respond to almost all vaccines more poorly than middle aged people. And we know that children often don’t respond well to vaccines because their immune responses aren’t fully developed for a while. But I would see no reason that this should have any different distribution across within the age groups, across ethnicities, country of origin, income or any of the other parameters. But I would say that the people who have put out the information have left that as an open possibility because we don’t have data for. And I think it’s a fair question for people to ask. I’ve given you what I hope the answer is, but we don’t have real data to show there any differences in ethnicities or any other category other than age.
Q: Would you be equally satisfied taking the Moderna or the Pfizer vaccine, personally?
BARRY BLOOM: I’m going to say something that I know sounds utterly self-serving and stupid, but I’ve made a commitment not to take a vaccine that can’t be taken by people in low income countries. So I’m going to wait till the vaccine prices come down, whether it’s the adenovirus vaccines or the Novavax vaccine, the price of which I don’t know. But if I took a vaccine, I’d want to be sure that everybody else in the world that wanted to and was medically able to take the vaccine could take a vaccine.
Q: Got it. About side effects, which you talked about earlier in this conversation or earlier in the session. How long do certain side effects last? Like if you get Bell’s palsy, which can be a serious condition. How long do these side effects last? Is it just hours or days or weeks?
BARRY BLOOM: So most of the arm pain, headache, muscle pain, joint pain, fatigue, clear by two days, occasionally three days, those are vaccine reactions, they’re expected and they go away. There are a couple of cases of Bell’s palsy, which is a problem on the facial nerves. Bell’s palsy, depending on how much damage to the nervous, you know, an adult’s nerves don’t regenerate very well. They’re often transient. And you can get over it, particularly if they’re appropriately treated to cut down on inflammation. And sometimes they’re permanent. But again, extremely rare.
Q: And in terms of the severe allergic reactions, I know you mentioned earlier that it’s very few people out of the sample that had severe allergic reactions. If you are one of those people who would have a severe allergic reaction. Are you going to be OK if you have an EpiPen or take an antihistamine?
BARRY BLOOM: Are you going to be OK? I can imagine circumstances where a reaction would be so great that you can only pump so much epinephrine in someone to relax the muscles in the throat. It’s like most medications, it doesn’t guarantee one hundred percent protection. Even in the adenovirus trial in AstraZeneca, when they gave antihistamines, they markedly reduced the vaccine reactions after the second dose, but they didn’t go away completely. So one would hope there were no reactions that required treatment. I would hope, and I believe the FDA recommendations may well be that all sites that deliver vaccines should have EpiPens available. So at least we could provide what we can provide in the cases of rare allergic reactions.
Q: Could there be very rare cases where there could be a fatal allergic reaction?
BARRY BLOOM: Absolutely. Ask people who have serious experience with these things to know how quickly you can have a bee sting and go into anaphylaxis, and in that circumstance, most people are protective if they carry around an EpiPen. But there are people lost the bee stings every year.
Q: And my last question is, do you have any guesstimate as to the timing of a childhood vaccine? You mentioned they haven’t tested yet on kids. I mean, is a childhood vaccine a year away? A few years away?
BARRY BLOOM: I can’t answer. I don’t think anybody can really answer that realistically, and the reason is there are many vaccines for kids in which you have to drop the dose, and that requires doing multiple dose trials, not necessarily randomized control for protection. But to be sure and I’m going to raise an important point that affects the timing. What is the tolerable dose for kids that may be much lower than it is for adults, that still generates a protective immune response? And that’s what the companies are going to have to do. They’ll be very lucky if they can give the same dose as adults because then they don’t have to change anything. It is quite possible they can’t and they will have to have as many vaccines to reduce the vaccines for children. And that requires reproduction, reformulation and all of the above. That’s going to take time. I have one high hope, this is my inevitable optimism, if it is definitively shown that if you have an antibody to the right piece of the spike protein, you are essentially guaranteed protection that becomes a biomarker or carpet of protection. You can run trials without looking for disease. You can say if the vaccine produces the same level of antibodies that we learn from trials, guarantees almost ninety five percent protection, that becomes an approvable vaccine regimen that the FDA has the prerogative to approve. That would save the necessity for constantly increasing trials of new vaccines, any new vaccine that could then target for a surrogate endpoint and say, if I make as many antibodies with my vaccine as they did with the first two vaccines, can I be able to have my vaccine if it’s shown to be safe in a large number of people? Can I now move that quickly without having to do thirty thousand people randomized, controlled? I’m optimistic. At some time, maybe by late spring or summer, the FDA will be asked to do that. And if the data are really strong and we don’t have those data now, that it is a sufficient condition for protection to have anti-spike antibodies of a certain kind. That would move things forward tremendously. And it would provide a test, by the way, of someone who had a vaccine or had an infection to know whether they have protective levels of anti-spike antibodies. That pretty much gives them a 95 percent chance of being protected.
Q: Thank you so much.
BARRY BLOOM: OK, everybody, thank you for your wonderful questions. I’m sorry for not so wonderful and overly long answers, but that’s the problem of a professor.
This concludes the December 16th press conference.