A long COVID researcher continues to search for answers

Amid federal funding cuts for health research, the Trump administration has shuttered the Department of Health and Human Services’ (HHS) Office of Long Covid Research and Practice. Beth Stelson, postdoctoral research fellow in the Department of Epidemiology, long COVID researcher, and herself a patient, discusses her research and the ramifications of the office’s closure.
What is long COVID and who is most at risk of getting it?
Long COVID is generally a constellation of symptoms that occur after someone has been infected with COVID-19. It can manifest as up to 200 or more different symptoms that can affect almost any organ in the body. Under the current definition, you usually can be considered to have long COVID if your symptoms have lasted for at least three months. We know that some people never recover or never go into remission. More severe COVID-19 infection increases your risk of long COVID. But since the majority of people around the world had mild cases—like myself—they constitute most of the people with long COVID, even though they had lower risk.
Given that long COVID encompasses so many different symptoms, does that make it hard to diagnose and to determine its prevalence?
Yes, that is part of the difficulty, as is awareness. There’s still a lot of misunderstanding around long COVID—for instance, some medical providers still misdiagnose it as a psychiatric condition. And some think you need a positive test for COVID to have a diagnosis, which is also not true. Providers can make a diagnosis based on somebody’s clinical history and how their symptoms have evolved.
At this point, it’s estimated that 6% to 7% of people who have acute COVID-19 infection will develop long COVID. The incidence was much higher at the start of the pandemic with the first strains of the COVID-19 virus, and many “first-wavers” still experience long COVID symptoms. The risk of developing long COVID has decreased with the later, weaker variants of the virus and the availability of vaccines, which is good news (and a reason for everybody to keep up-to-date with their COVID vaccines). But studies have also found that the more times you get COVID, the greater the likelihood that you could develop long COVID, which is really important to know since many people no longer take the weaker variants as seriously. In addition, people can have long COVID and their symptoms can go into remission, and if they get COVID again, those symptoms can reemerge. So long COVID is very much a real public health concern today, as it was at the very beginning. It affects hundreds of millions of people around the world.
How is long COVID treated?
Since long COVID symptoms vary widely, so do treatments. Right now, there’s no cure. There are some ways to manage symptoms. So, for example, someone could work with a pulmonologist to manage lung-related symptoms. But I think what is particularly difficult about long COVID for patients is that it can affect so many different organs. And our medical systems are set up based on individual organ systems and not necessarily on diseases that affect multiple systems. So the burden to coordinate care falls on patients who have the least amount of energy to be able to do that.
Long COVID clinics tend to be located in urban areas, often around academic medical centers, so access to care, especially for people who live in rural areas, is substantially lower.
Can you describe your long COVID research?
I’m involved with the Patient-Led Research Collaborative (PLRC), a group of about 60 researchers and health advocates from across the globe living with long COVID and other infection-associated chronic conditions. We aim to improve research into long COVID and to improve life for those with the condition. PLRC did the first study on long COVID symptoms. A friend forwarded me their survey and said “Hey, this sounds like what you have!” After I took the survey, I immediately reached out and asked how I could be a part of it.
I’m a workplace researcher who has conducted research on returning to work with long COVID. How do we support individuals with long COVID to remain engaged and lead in the workplace? If we can’t figure this out, we risk having a large component of our society being excluded from jobs and from economic engagement.
One study I worked on as part of the PLRC was a qualitative study on return to work among long COVID patients. We found that participants expressed a strong desire and need to return to work, motivated by a sense of purpose and financial precarity. They also described how fluctuating symptoms, exacerbated by work-related tasks, made returning challenging and how being able to work relied on receiving job accommodations and support. Non-work factors were also important, such as receiving a long COVID medical diagnosis and having help at home. Many participants said there were barriers to accessing both work and non-work supports, showing the pervasiveness of stigma and disbelief in long COVID as a medical condition.
Another study looked at the risk of psychiatric conditions in long COVID patients which, like other chronic conditions, increases the risk of mental health challenges. We found that a substantial minority of long COVID patients experienced suicidality, depression, and anxiety symptoms. Worse mental health was linked with factors such as more severe long COVID symptoms, financial hardship, and disbelief about the symptoms, while supportive responses from family, friends, and medical providers reduced reported mental health challenges.
Where does research on the condition stand overall?
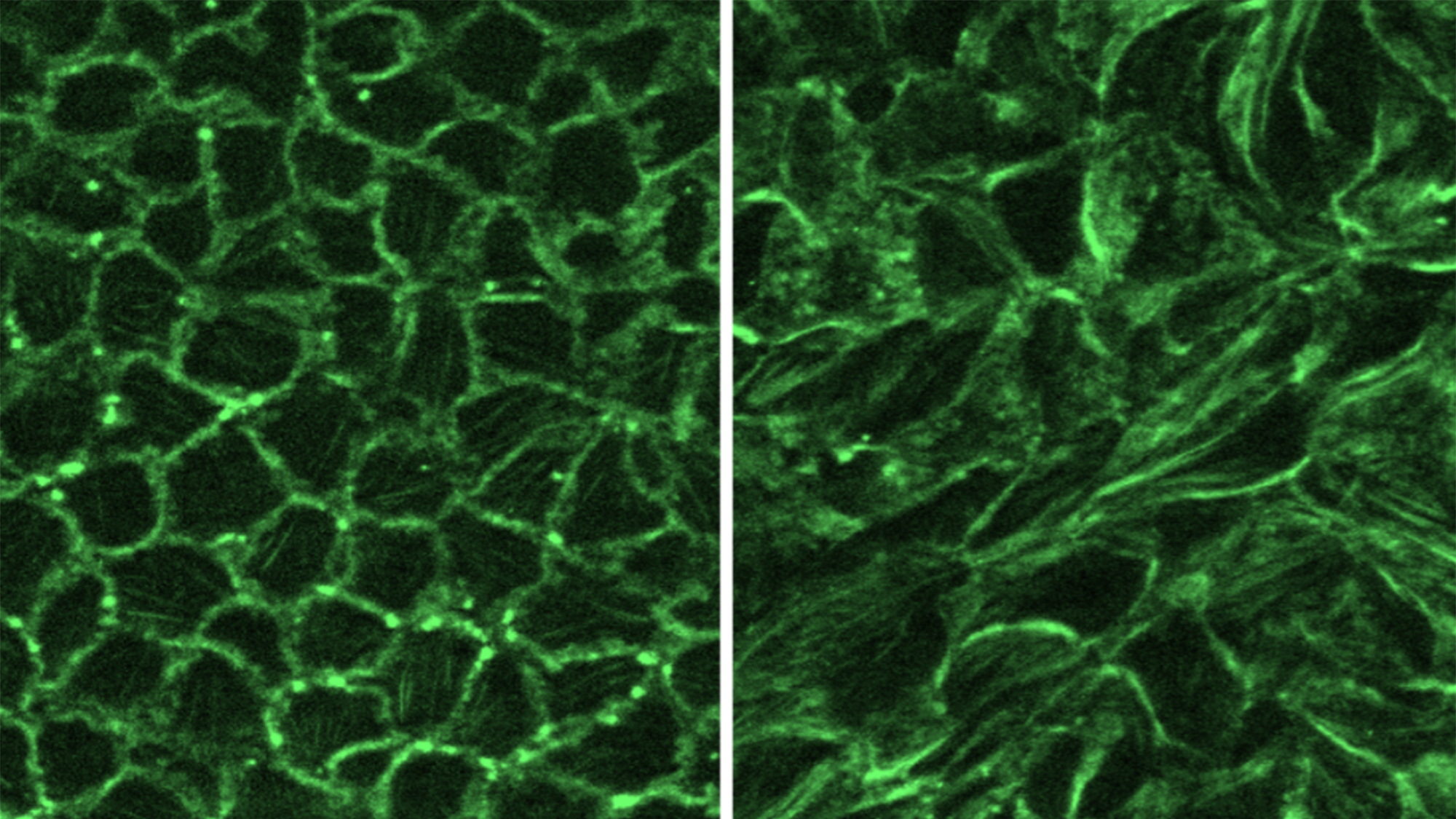
We’ve made huge headway in understanding the pathophysiology of how this condition can develop and have uncovered similarities with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia, which are also conditions that are often overlooked in health care. Other research has come out on the economic burden of this condition, to help marshal the business argument for why this research is important. And I think PLRC has demonstrated that including patients and community members in research is not ancillary, it’s essential in improving study design, interpretation, and dissemination.
What would you like to see going forward?
I’d like to see more investment in clinical trials to test treatments. We also need to invest in long-term cohorts so we can study patients over time.
Also, I think we need to invest in research about how to keep people, whether they have long COVID or other disabilities, not just engaged in the workforce, but also how to give them opportunities to lead in the workforce and to have more say in the design of the work environment. Our work environments are currently designed around employers, but we need them to be designed around workers who inevitably will get sick, have caregiving responsibilities, and will age. Reducing documentation required to access accomodations, iterative return-to-work processes, and flexible work arrangements are all key.
What are the ramifications of the closing of the Office of Long COVID Research and Practice?
Just like long COVID affects many different parts of the body, it also affects many different parts of our lives, our communities, our economy. We need a holistic approach, a coordinating body to help advance care, treatment, and social supports for the long COVID community. The mission of the Office of Long COVID Research and Practice was to be this coordinating body, and the establishment of this office was hard fought by patients. So it feels like a kick in the gut to have it closed at a time when we have really put long COVID on the map as a condition and as a health care and public health crisis.
We need more awareness around long COVID, not less. By taking away this office that’s supposed to advance research and practice, you’re taking away opportunities for progress. You’re taking away hope from many people. I fear there will be very real health consequences for our communities.
Fatigue, migraines, fevers, and stigma
Beth Stelson describes her experience with long COVID
I was in the first wave of people who developed long COVID. On March 14, 2020, Harvard shut down and went remote. My spouse was living in Florida at the time. He came up and got sick the next day. I got sick after him and didn’t get better. I had relapsing and remitting symptoms including post-exertional malaise, rapid heartbeat, migraines, neuropathy in my toes, fevers that would spike and then go away. We weren’t sure if I was continuing to get re-infected or what was going on until stories about patterns of these long-term symptoms began emerging in the media.
Since then, I’ve experienced stigma with care providers, pretty much saying that my symptoms are based on anxiety and stress. One cardiologist told me that I should have a plant-based diet—even though I’ve been a vegetarian since I was 15. The suggestion was that symptoms I’ve experienced, such as my wildly fluctuating blood pressure and brain fog were triggered by my own mental health—which was not the case.
In my third year living with long COVID I got pregnant. While I didn’t experience any stigma from my ob-gyn, she told me she didn’t know anything about the condition. There is so little research on long COVID and pregnancy or research specific to menstruating people, and not being able to access the support and information that I needed made me feel very vulnerable as a patient.
My symptoms have gradually improved over the first three years following my first bout with COVID and then plateaued with the birth of my child. I’m doing a lot better these days. I consider myself to be mostly in remission. However, I have noticed that they reeemerge when I get reinfected with COVID or with other viral illnesses such as RSV, so I now take great care to avoid all viral illness (which of course is so hard to do having a toddler).
There is a lot of stigma in the workplace—including in academia—about sharing when you have a chronic condition or need help since there is so much emphasis on productivity. This experience has informed my understanding of disability justice, especially in the workplace, and I now try to bring this to my occupational health research. I think it’s important to share experiences of when we need help so we can have more conversation and recognize the diversity and fluctuation of work needs over time.