Obesity

[contentarea class=”obesity-opener”]
Special Report—Spring 2017
by Madeline Drexler
Editor, Harvard Public Health
2018 CASE Circle of Excellence Silver Award in Topical Feature Writing
Have you ever looked at old photos from 1970s protest marches? Feminists demanding the Equal Rights Amendment, environmentalists calling for clean air and water, gay liberation, the Black Panthers, the Chicano movement, on and on: In each case, committed and strategically canny people translated personal and group experiences of injustice into the mobilizing power of the collective.
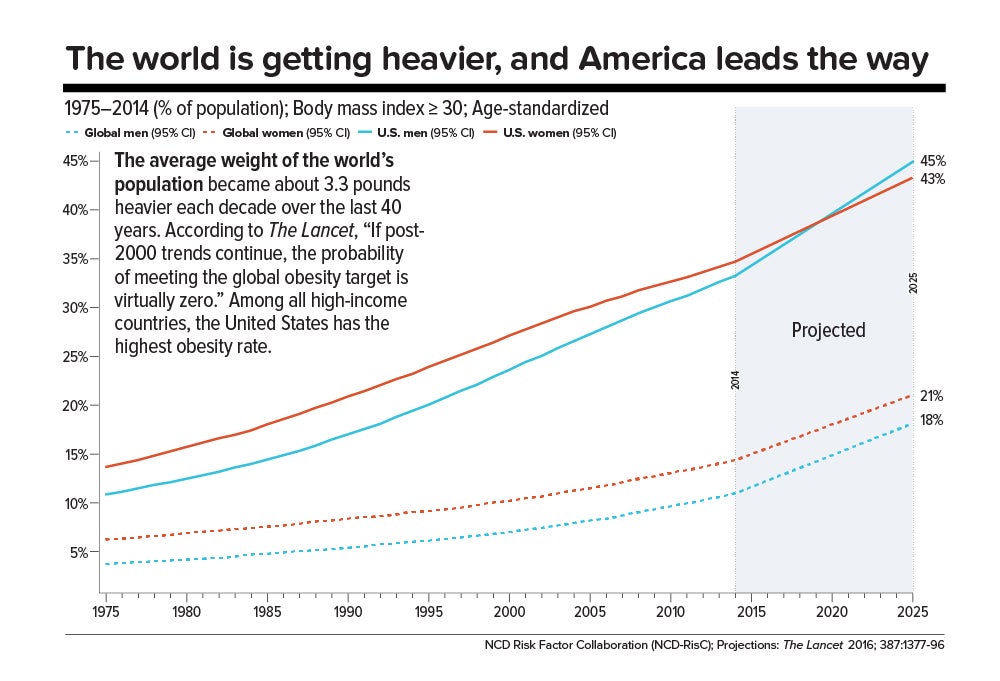
Look closer at the photos. Just as arresting as the fashions and the hairstyles and the palpable air of urgency around still-urgent issues is another detail: To contemporary eyes, people look thin. We now know that in the United States in the 1970s, two public health crises were germinating. One was HIV/AIDS, the victims of which were consigned to the shadows until activism forced changes in research funding, medical protocols, and social attitudes.
The other crisis was an unprecedented obesity epidemic that has never reversed course. It was incited not by a sudden wave of individual gluttony (even toddlers are afflicted) but by a radical and toxic change in our food environment. The public health establishment spent decades leaning on people to change their behavior. Today, researchers are beginning to wonder if it’s time for an entirely different approach.
Might that new approach draw on the defiant energy of other social movements of the last 40 years?
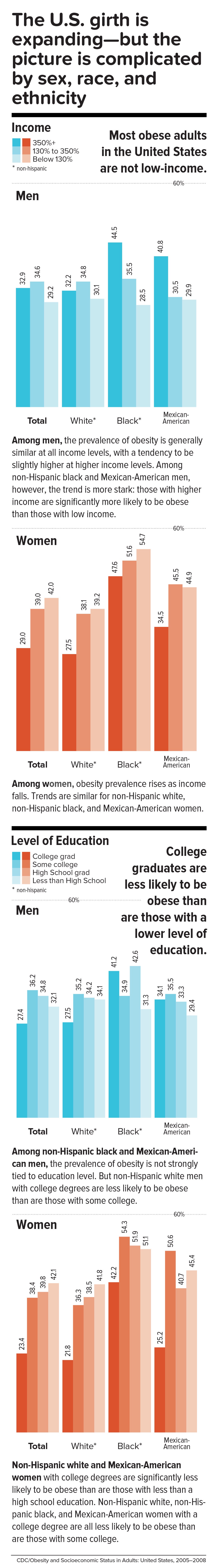
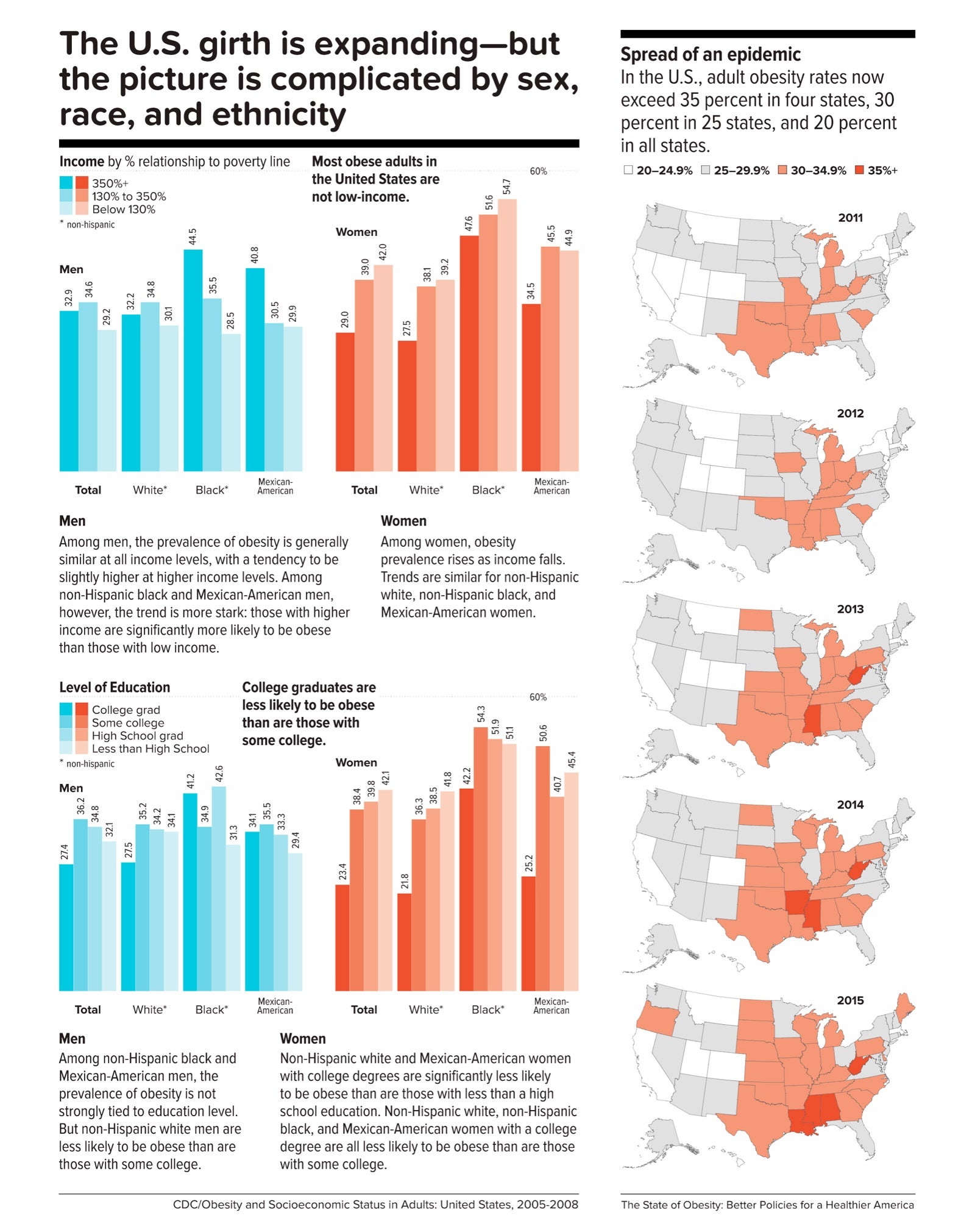
Statistics obscure suffering
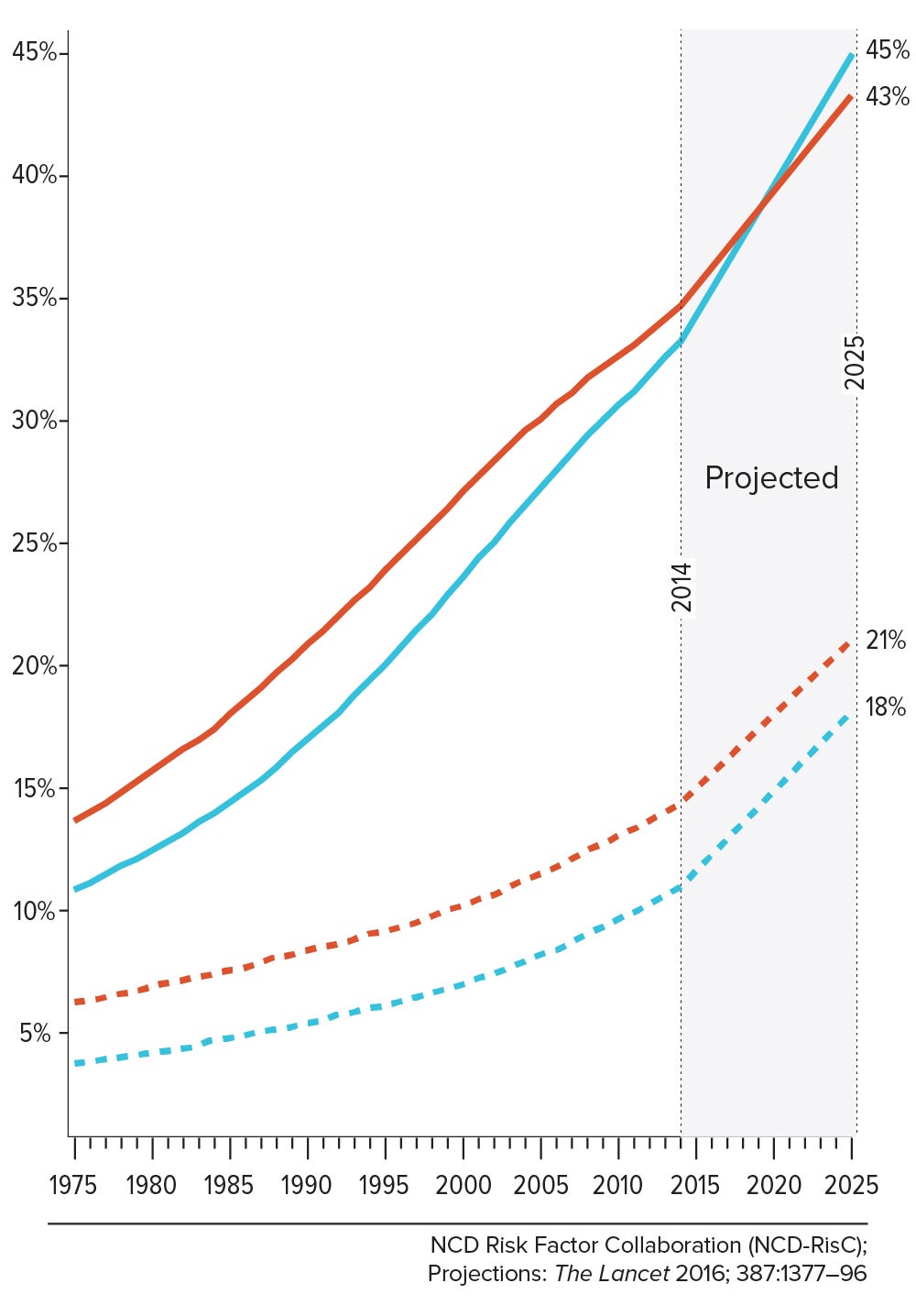
According to 2014 national data, 35 percent of adult men and 40.4 percent of adult women are obese—that is, their body mass index, or BMI, a standard calculation of weight divided by height, is greater than or equal to 30. (Normal BMI is 18.5 to 24.9; overweight is 25 to 29.9.) Among youth 2 to 19 years old, the prevalence of obesity is 17 percent, and extreme obesity (a BMI at or above 120 percent of the 95th percentile on standard child growth charts), 5.8 percent. All told, more than 70 percent of Americans ages 20 and over are either overweight or obese.
It is not a matter of benign padding. Compared with those with a normal or healthy weight, people who are obese face increased risk for dying of all causes and, more specifically, for suffering cardiovascular disease, type 2 diabetes, stroke, osteoarthritis, sleep apnea, certain cancers (20 percent of cancers in women and 16 percent in men are related to obesity), depression and anxiety, and many other chronic health complications.
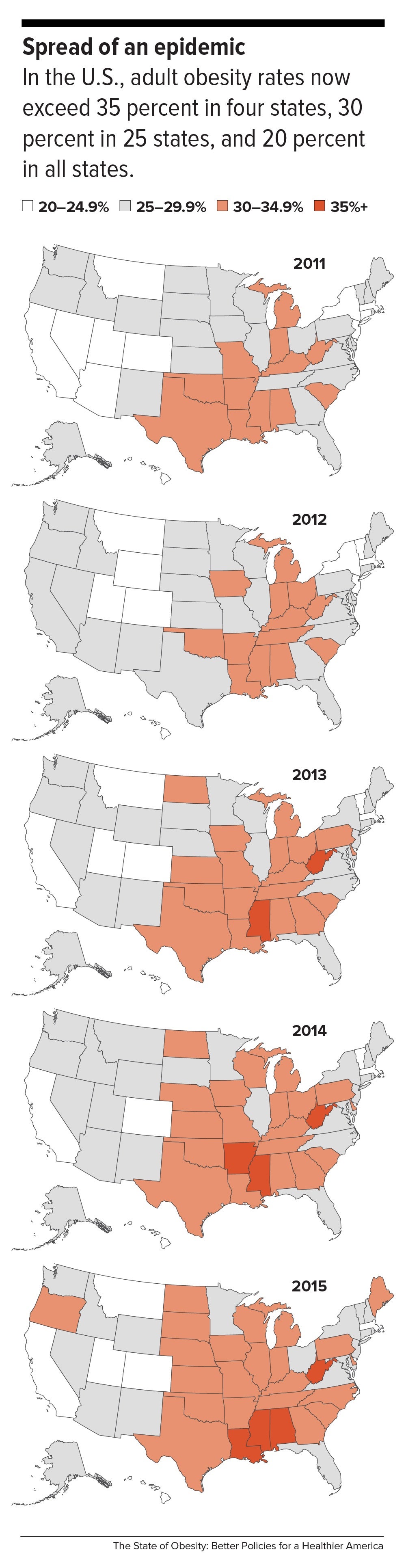
Mounting research, including a 2016 study in the Journal of the American Medical Association (JAMA), suggests that U.S. life expectancy may be starting to decline—the first time since 1993, when HIV-related deaths were peaking. Age-adjusted death rates for the first nine months of 2015 rose sharply compared with the same period in 2014—and, most notably, involved causes of death linked to obesity. If this trajectory continues, the health complications of obesity in America will soon eclipse the benefits from declines in smoking.
How did we get here?
In 1987, Steven Gortmaker, Harvard Chan professor of the practice of health sociology, co-authored a study in the American Journal of Diseases of Children that sounded an alarm. Between 1963 and 1980, among children ages 6 to 11, there was a 54 percent increase in the prevalence of obesity and a 98 percent increase in what was then called superobesity. This wasn’t the first clue that something was wrong. A 1985 study by Gortmaker and colleagues had documented a link between child obesity and television viewing (mainly through exposure to ads). These early warnings of an impending epidemic were followed by rapid increases in the prevalence of obesity across older age groups.
But not until 1999, when JAMA devoted an entire issue to the topic, did obesity hit the headlines as a bona fide threat to public health, not merely a personal cosmetic problem. As another article in the same issue noted, “Rarely do chronic conditions such as obesity spread with the speed and dispersion characteristic of a communicable disease epidemic.”
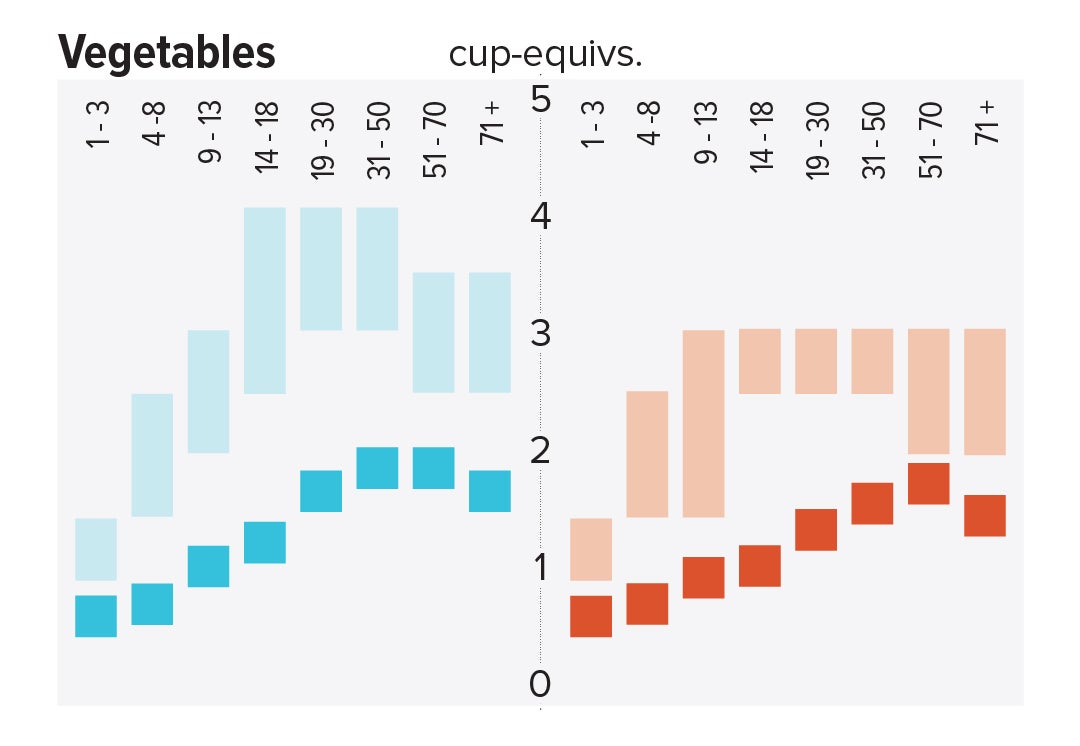
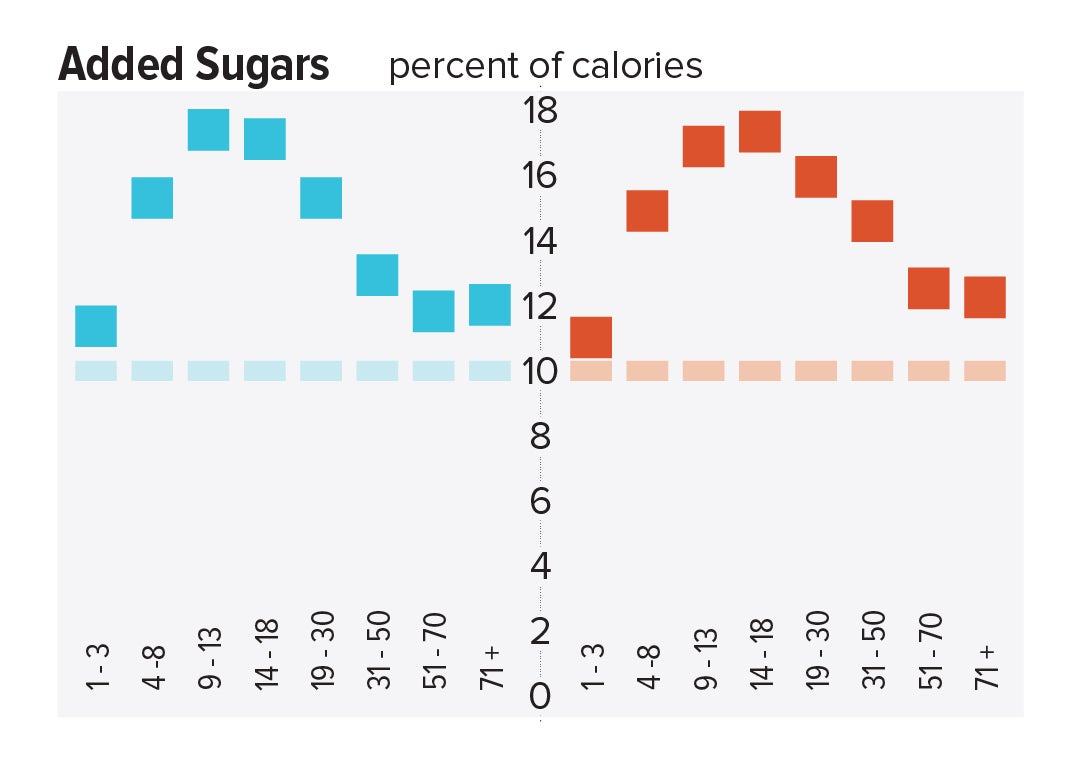
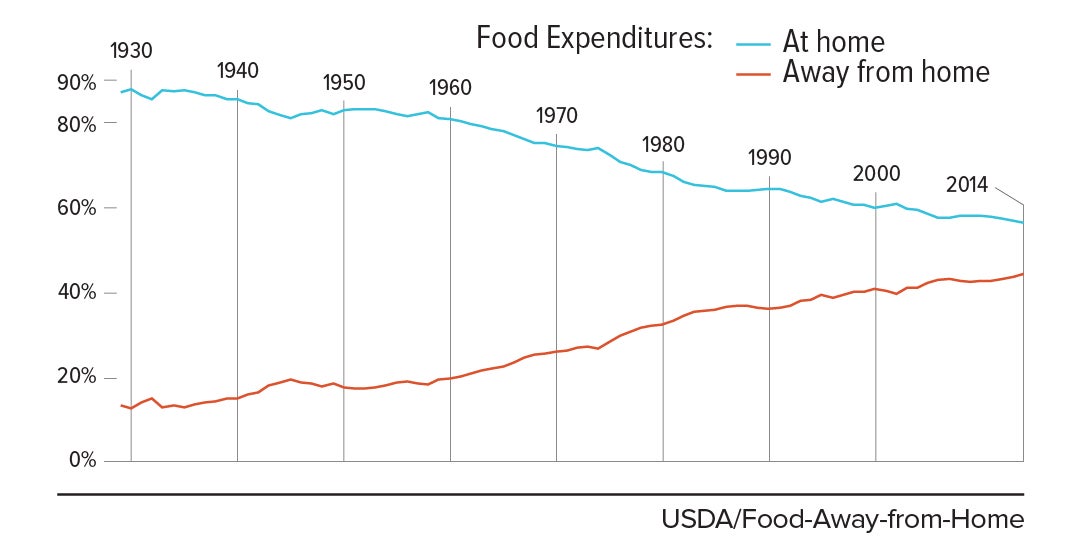
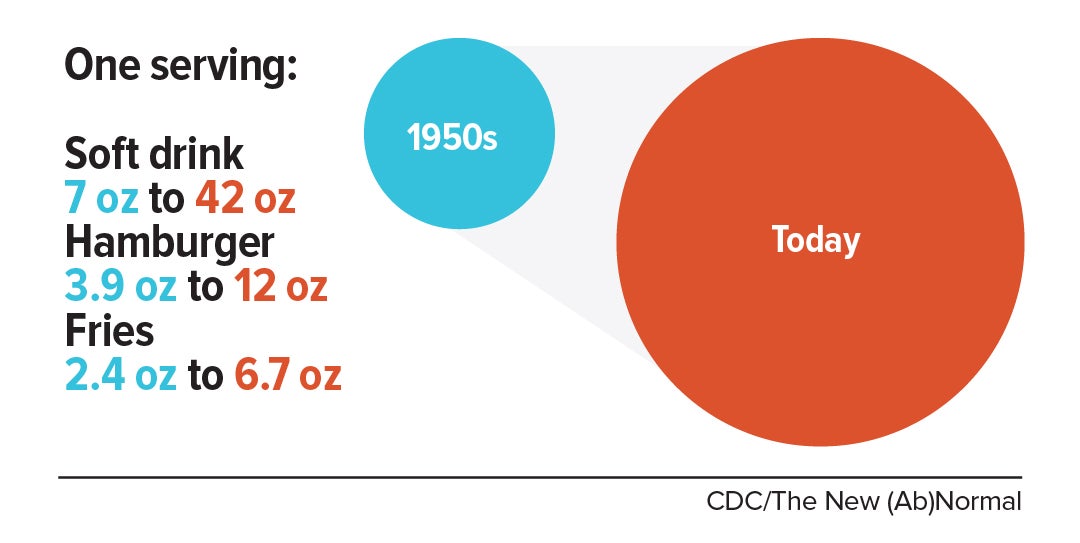
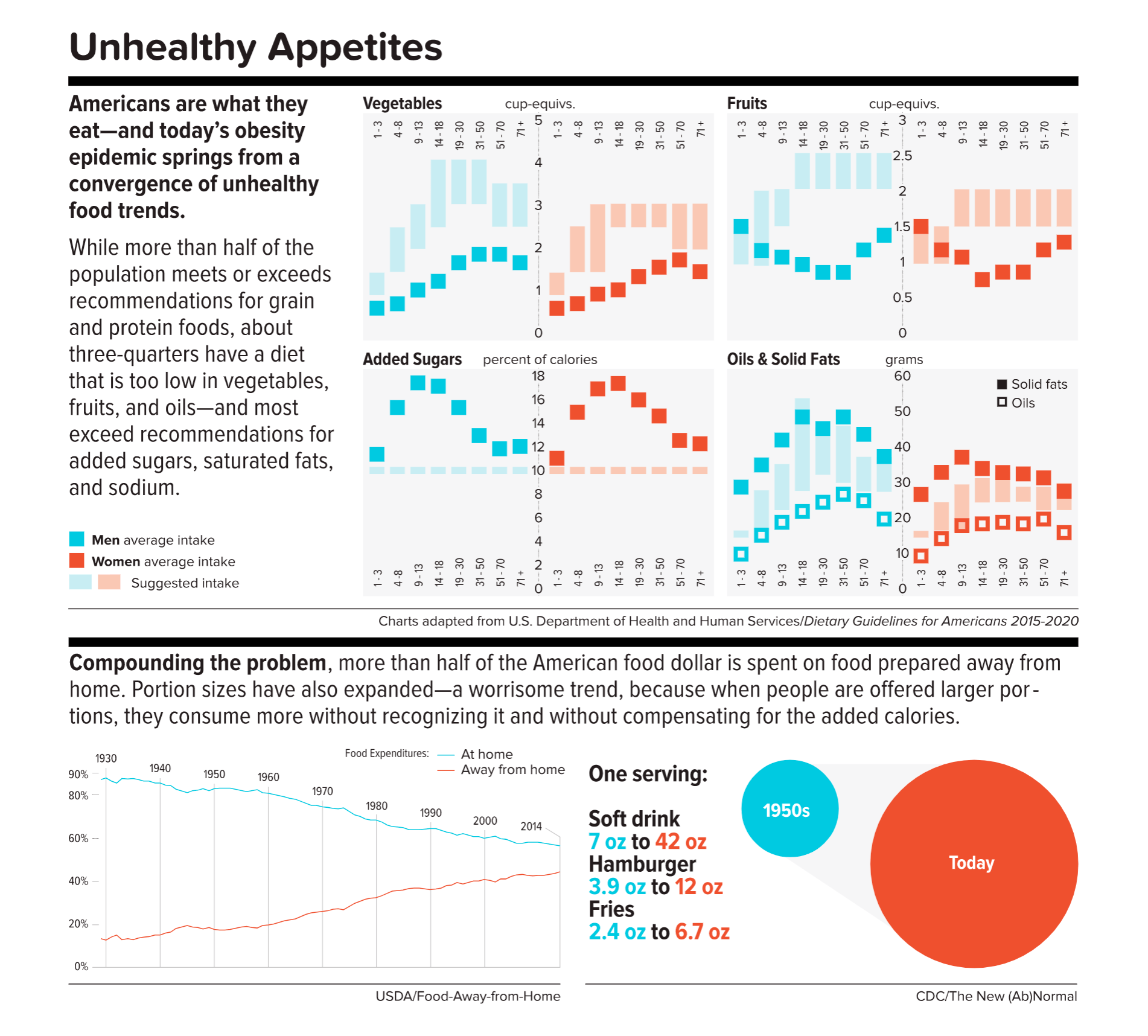
While the reasons for skyrocketing obesity were largely elusive 30 years ago, they are obvious now. The modern food era has spread out a smorgasbord of hyperpalatable, flavor-enhanced, additive-laced, convenient, and relatively affordable foods that are high in added sugar, unhealthy fats, and salt, and engineered to overcome our internal homeostatic eating signals. Our bodies and brains are all but helpless in response.
Nutritionist and food industry critic Marion Nestle wrote in her book Food Politics that a convergence of business and marketing has “encouraged us to eat more food, more often, in more places.” In a culture that continually amps up our desire for food, many Americans believe this disordered pattern of consumption is our birthright; until recently, we have displayed little appetite for government interference.
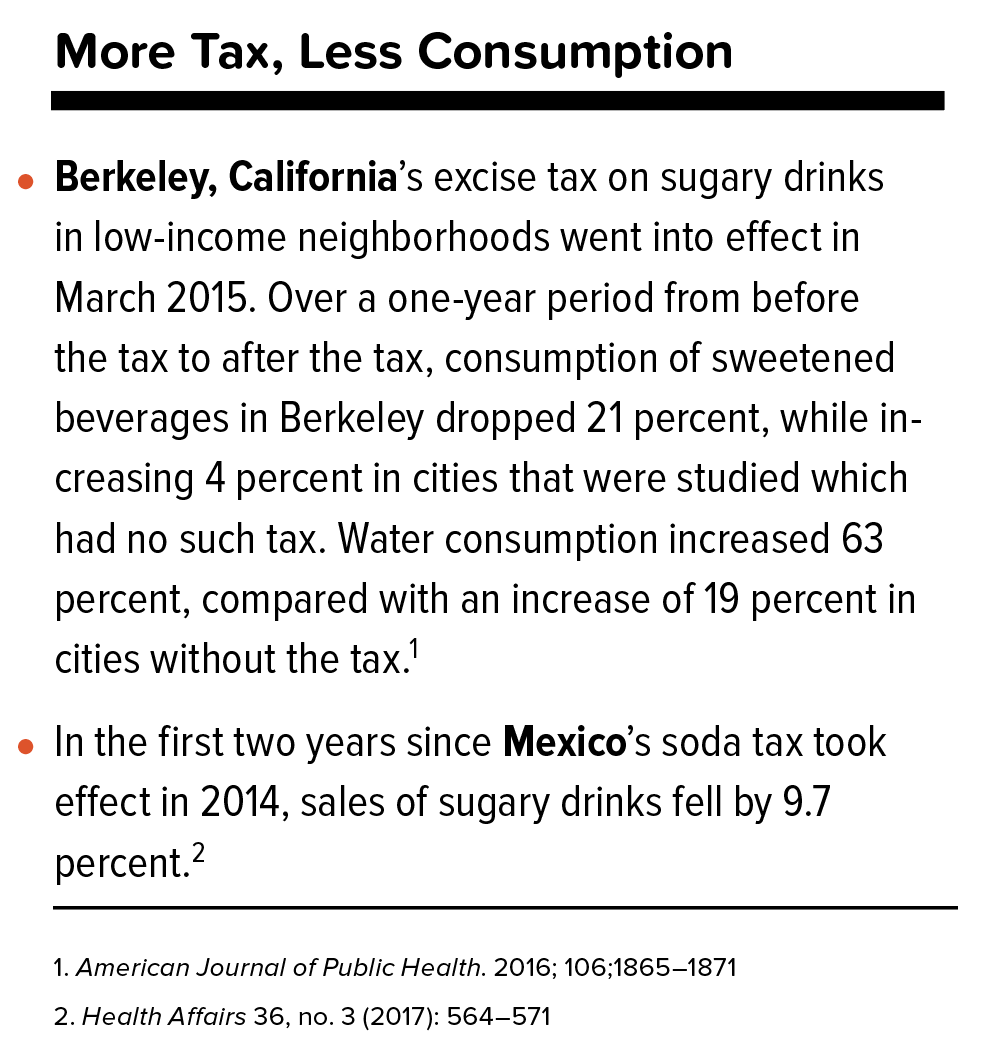
While weight is, of course, partly a matter of personal responsibility, America’s obesity epidemic is mainly driven by upstream influences from industry, federal policies, and social norms. Today, people are beginning to perceive those upstream forces. Consider: Since 2014, voters in seven U.S. cities or counties have approved taxes on sugar-sweetened beverages—a move that would have been inconceivable five years ago—and a slew of proposals for even higher excise taxes on these nutritionally empty refreshments are in the works all across the country. Sales of fast food, sugary drinks, and pizza are all flagging. Industry is scaling back junk food ads to children and also scaling back sugar in the products peddled on Saturday mornings. Children’s school lunches are healthier than ever. Restaurants are tweaking recipes in the direction of virtue. The Panera Bread Company recently became the first major chain to list the amount of added sugars in its fountain beverages. And in March, the industry consulting firm Beverage Marketing Corporation announced that, in 2016, for the first time, Americans guzzled more bottled water than soda.
“This is a turning point on several important fronts,” says Kelly Brownell, dean of the Sanford School of Public Policy at Duke University and a leading expert on the food industry’s contribution to the obesity trend. “The country has given government permission to act in ways that make the nutrition landscape more healthy.” Still, the gains are tenuous, in part because of industry muscle and a current distaste for regulation in Washington, DC.
So what would it take to sustain the nascent progress? In 2017, what would an inspired agenda to halt the obesity epidemic look like?
It might look like this.
[/contentarea]
1.
Prevention, prevention, prevention.
Losing weight is hard to do.
In the U.S., only one in six adults who have dropped excess pounds actually keep off at least 10 percent of their original body weight. The reason: a mismatch between biology and environment. Our bodies are evolutionarily programmed to put on fat to ride out famine and preserve the excess by slowing metabolism and, more important, provoking hunger. People who have slimmed down and then regain their weight don’t lack willpower—their bodies are fighting them every inch of the way.
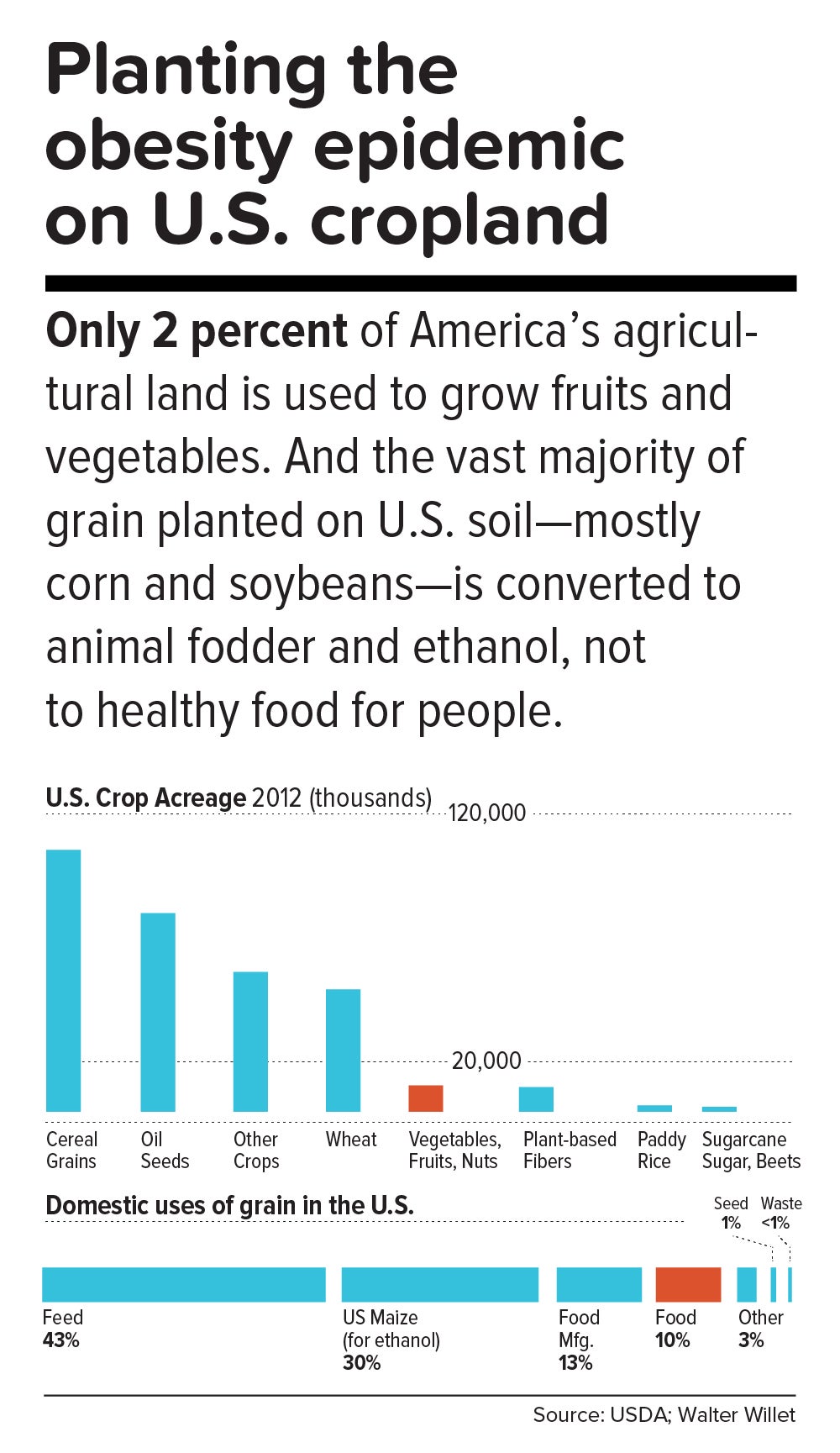
[sidebar class=”ob-graphic” position=”right” offset=”true”]
[/sidebar]
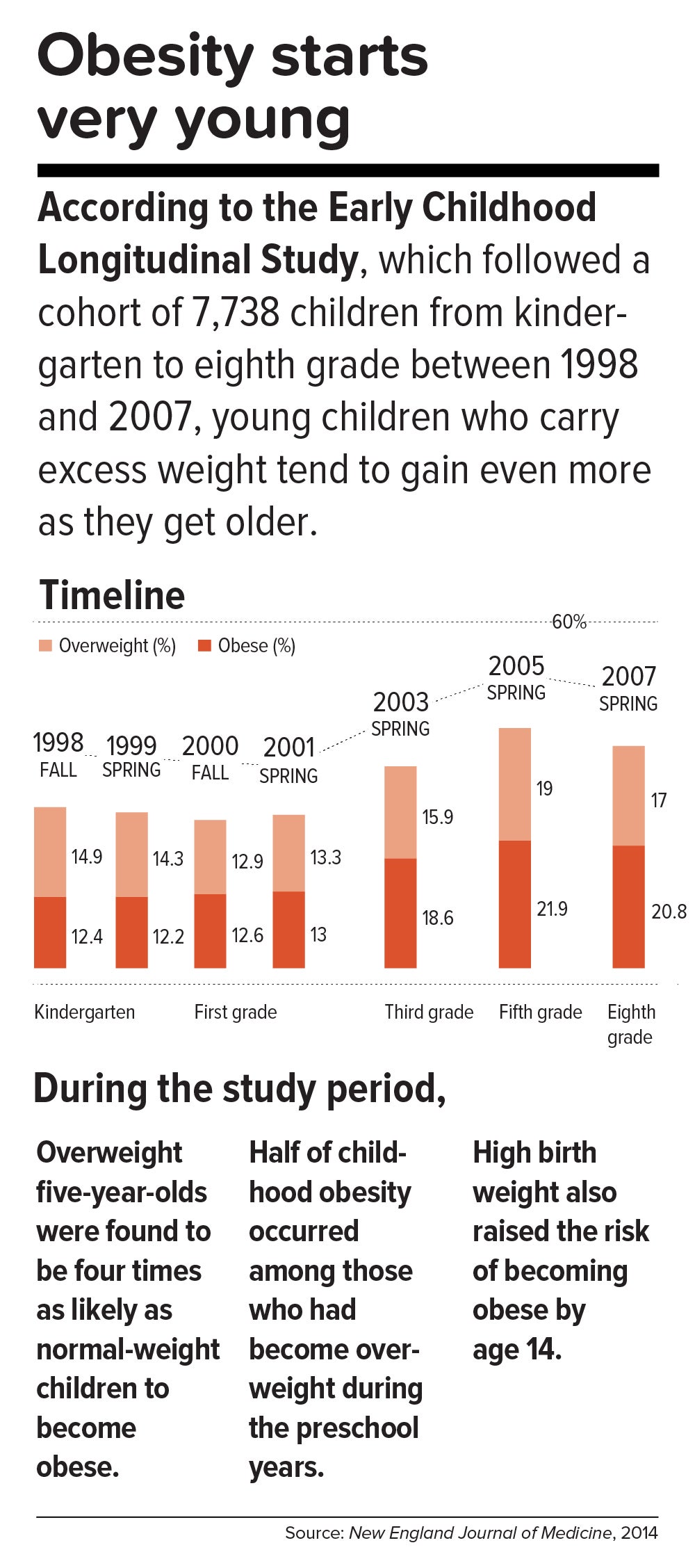
This inborn predisposition to hold on to added weight reverberates down the life course. Few children are born obese, but once they become heavy, they are usually destined to be heavy adolescents and heavy adults. According to a 2016 study in the New England Journal of Medicine, approximately 90 percent of children with severe obesity will become obese adults with a BMI of 35 or higher. Heavy young adults are generally heavy in middle and old age. Obesity also jumps across generations; having a mother who is obese is one of the strongest predictors of obesity in children.
All of which means that preventing child obesity is key to stopping the epidemic. By the time weight piles up in adulthood, it is usually too late. Luckily, preventing obesity in children is easier than in adults, partly because the excess calories they absorb are minimal and can be adjusted by small changes in diet—substituting water, for example, for sugary fruit juices or soda.
Still, the bulk of the obesity problem—literally—is in adults. According to Frank Hu, chair of the Harvard Chan Department of Nutrition, “Most people gain weight during young and middle adulthood. The weight-gain trajectory is less than 1 pound per year, but it creeps up steadily from age 18 to age 55. During this time, people gain fat mass, not muscle mass. When they reach age 55 or so, they begin to lose their existing muscle mass and gain even more fat mass. That’s when all the metabolic problems appear: insulin resistance, high cholesterol, high blood pressure.”
Adds Walter Willett, Frederick John Stare Professor of Epidemiology and Nutrition at Harvard Chan, “The first 5 pounds of weight gain at age 25—that’s the time to be taking action. Because someone is on a trajectory to end up being 30 pounds overweight by the time they’re age 50.”
The most realistic near-term public health goal, therefore, is not to reverse but rather to slow down the trend—and even this will require strong commitment from government at many levels. In May 2017, the Trump administration rolled back recently-enacted standards for school meals, delaying a rule to lower sodium and allowing waivers for regulations requiring cafeterias to serve foods rich in whole grains. If recent expansions in food entitlements and school meals are undermined, “It would be a ‘disaster,’ to use the president’s word,” says Marlene Schwartz, director of the Rudd Center for Obesity & Food Policy at the University of Connecticut. “The federal food programs are incredibly important, not just because of the food and money they provide families, but because supporting better nutrition in child care, schools, and the WIC [Women, Infants, and Children] program has created new social norms. We absolutely cannot undo the progress that we’ve made in helping this generation transition to a healthier diet.”
[contentarea class=”obesity-section-2″]
Federal obesity-fighting policies we can’t afford to lose
Healthy, Hunger-Free Kids Act
The 2010 legislation established strong national nutrition standards for all food sold in schools, including in vending machines and school stores, and increased the number of eligible children enrolled in school meals programs. The centerpiece of former first lady Michelle Obama’s Let’s Move! campaign, the law was implemented in 2012.
Special Supplemental Nutrition Program for Women, Infants and Children (WIC)
In 2009, the WIC program expanded to cover fresh fruits, vegetables, and whole grains, the first major change to the program since the 1970s.
Nutrition Labeling of Standard Menu Items at Chain Restaurants
Part of the 2010 Affordable Care Act, the law was slated to go into effect on May 5 of this year. It requires all chain restaurants, supermarkets, convenience stores, and movie theaters with 20 or more outlets nationally to provide calorie information on menus and menu boards. In anticipation of the new policy, numerous venues have reformulated their fare with healthier ingredients.
[/contentarea]
2.
Get the science right.
It is impossible to prescribe solutions to obesity without reminding ourselves that nutrition scientists botched things decades ago and probably sent the epidemic into overdrive. Beginning in the 1970s, the U.S. government and major professional groups recommended for the first time that people eat a low-fat/high-carbohydrate diet. The advice was codified in 1977 with the first edition of The Dietary Goals for the United States, which aimed to cut diet-related conditions such as heart disease and diabetes. What ensued amounted to arguably the biggest public health experiment in U.S. history, and it backfired.
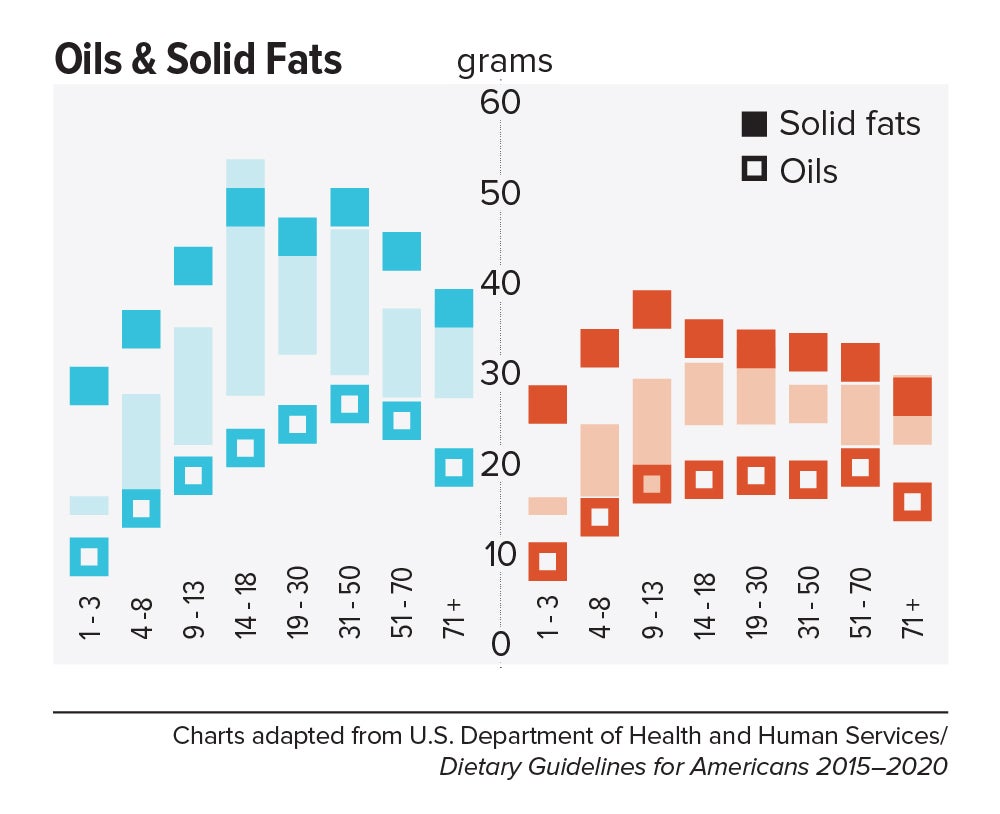
At the time, saturated fat and dietary cholesterol were believed to be the main factors responsible for cardiovascular disease—an oversimplified theory that ignored the fact that not all fats are created equal. Soon, the public health blitz against saturated fat became a war on all fat. In the American diet, fat calories plummeted and carb calories shot up.
“We can’t blame industry for this. It was a bandwagon effect in the scientific community, despite the lack of evidence—even with evidence to the contrary,” says Willett. “Farmers have known for thousands of years that if you put animals in a pen, don’t let them run around, and load them up with grains, they get fat. That’s basically what has been happening to people: We created the great American feedlot. And we added in sugar, coloring, and seductive promotion for low-fat junk food.”
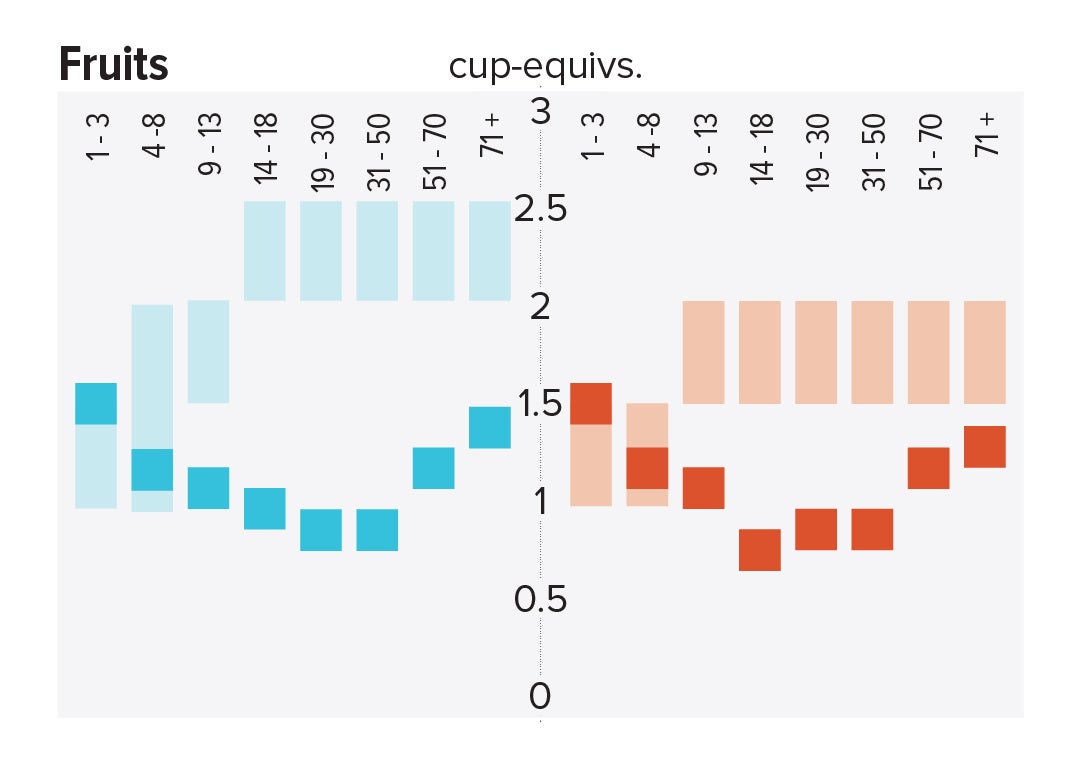
Scientists now know that whole fruits and vegetables (other than potatoes), whole grains, high-quality proteins (such as from fish, chicken, beans, and nuts), and healthy plant oils (such as olive, peanut, or canola oil) are the foundations of a healthy diet.
But there is also a lot scientists don’t yet know. One unanswered question is why some people with obesity are spared the medical complications of excess weight. Another concerns the major mechanisms by which obesity ushers in disease. Although surplus body weight can itself directly cause problems—such as arthritis due to added load on joints, or breast cancer caused by hormones secreted by fat cells—in general, obesity triggers myriad biological processes. Many of the resulting conditions—such as atherosclerosis, diabetes, and even Alzheimer’s disease—are mediated by inflammation, in which the body’s immune response becomes damagingly self-perpetuating. In this sense, today’s food system is as inflammagenic as it is obesigenic.
Scientists also need to ferret out the nuanced effects of particular foods. For example, do fermented products—such as yogurt, tempeh, or sauerkraut—have beneficial properties? Some studies have found that yogurt protects against weight gain and diabetes, and suggest that healthy live bacteria (known as probiotics) may play a role. Other reports point to fruits being more protective than vegetables in weight control and diabetes prevention, although the types of fruits and vegetables make a difference.
A 2017 article in the American Journal of Clinical Nutrition showed that substituting whole grains for refined grains led to a loss of nearly 100 calories a day—by speeding up metabolism, cutting the number of calories that the body hangs on to, and, more surprisingly, by changing the digestibility of other foods on the plate. That extra energy lost daily—by substituting, say, brown rice for white rice or barley for pita bread—was equivalent to a brisk 30-minute walk. One hundred calories a day, sustained over years, and multiplied by the population is one mathematical equivalent of the obesity epidemic.
A companion study found that adults who ate a whole-grain-rich diet developed healthier gut bacteria and improved immune responses. That particular foods alter the gut microbiome—the dense and vital community of bacteria and other microorganisms that work symbiotically with the body’s own digestive system—is another critical insight. The microbiome helps determine weight by controlling how our bodies extract calories and store fat in the liver, and the microbiomes of obese individuals are startlingly efficient at harvesting calories from food. [To learn more about Harvard Chan research on the gut microbiome, read “Bugs in the System.”] The hormonal effects of sleep deprivation and stress—two epidemics concurrent and intertwined with the obesity trend—are other promising avenues of research.
And then there are the mystery factors. One recent hypothesis is that an agent known as adenovirus 36 partly accounts for our collective heft. A 2010 article in The Royal Society described a study in which researchers examined samples of more than 20,000 animals from eight species living with or around humans in industrialized nations, a menagerie that included macaques, chimpanzees, vervets, marmosets, lab mice and rats, feral rats, and domestic dogs and cats. Like their Homo sapiens counterparts, all of the study populations had gained weight over the past several decades—wild, domestic, and lab animals alike. The chance that this is a coincidence is, according to the scientists’ estimate, 1 in 10 million. The stumped authors surmise that viruses, gene expression changes, or “as-of-yet unidentified and/or poorly understood factors” are to blame.
3.
Master the art of persuasion.
A 2015 paper in the American Journal of Public Health revealed the philosophical chasm that hampers America’s progress on obesity prevention. It found that 72 to 98 percent of obesity-related media reports emphasize personal responsibility for weight, compared with 40 percent of scientific papers.
A recent study by Drexel University researchers also quantified the political polarization around public health measures. From 1998 through 2013, Democrats voted in line with recommendations from the American Public Health Association 88.3 percent of the time, on average, while Republicans voted for the proposals just 21.3 percent of the time.
Clearly, we can’t count on bipartisan goodwill to stem the obesity crisis. But we can ask what kinds of messages appeal to politically divergent audiences. A stealth strategy may be to avoid even uttering the word “obesity.” On January 1 of this year, Philadelphia’s 1.5-cents-per-ounce excise tax on sugar-sweetened and diet beverages took effect. When Philadelphia Mayor Jim Kenney lobbied voters to approve the tax, his bid centered not on improving health—the unsuccessful pitch of his predecessor—but on raising $91 million annually for prekindergarten programs.
“That’s something lots of people care about and can get behind—it’s a feel-good policy, and it makes sense,” says psychologist Christina Roberto, assistant professor of medical ethics and health policy at the University of Pennsylvania, and a former assistant professor of social and behavioral sciences and nutrition at Harvard Chan. The provision for taxing diet beverages was also shrewd, she adds, because it spread the tax’s pain; since wealthier people are more likely than less-affluent individuals to buy diet drinks, the tax could not be slapped with the label “regressive.”
But Roberto sees a larger lesson in the Philadelphia story. Public health messaging that appeals to values that transcend the individual is less fraught, less stigmatizing, and perhaps more effective. As she puts it, “It’s very different to hear the message, ‘Eat less red meat, help the planet’ versus ‘Eat less red meat, help yourself avoid saturated fat and cardiovascular disease.’”
Supermarket makeovers
Supermarket aisles are other places where public health can shuffle a deck stacked against healthy consumer choices.
With slim profit margins and 50,000-plus products on their shelves, grocery stores depend heavily on food manufacturers’ promotional incentives to make their bottom lines. “Manufacturers pay slotting fees to get their products on the shelf, and they pay promotion allowances: We’ll give you this much off a carton of Coke if you put it on sale for a certain price or if you put it on an end-of-aisle display,” says José Alvarez, former president and chief executive officer of Stop & Shop/Giant-Landover, now senior lecturer of business administration at Harvard Business School. Such promotional payments, Alvarez adds, often exceed retailers’ net profits.
Healthy new products—like flash-frozen dinners prepared with heaps of vegetables and whole grains, and relatively little salt—can’t compete for prized shelf space against boxed mac and cheese or cloying breakfast cereals. One solution, says Alvarez, is for established consumer packaged goods companies to buy out what he calls the “hippie in the basement” firms that have whipped up more nutritious items. The behemoths could apply their production, marketing, and distribution prowess to the new offerings—and indeed, this has started to happen over the last five years.
Another approach is to make nutritious foods more convenient to eat. “We have all of these cooking shows and upscale food magazines, but most people don’t have the time or inclination—or the skills, quite frankly—to cook,” says Alvarez. “Instead, we should focus on creating high-quality, healthy, affordable prepared foods.”
An additional model is suggested by Jeff Dunn, a 20-year veteran of the soft drink industry and former president of Coca-Cola North America, who went on to become an advocate for fresh, healthy food. Dunn served as president and chief executive officer of Bolthouse Farms from 2008 to 2015, where he dramatically increased sales of baby carrots by using marketing techniques common in the junk food business. “We operated on the principles of the three 3 A’s: accessibility, availability, and affordability,” says Dunn. “That, by the way, is Coke’s more-than-70-year-old formula for success.”
[contentarea class=”obesity-section-1″]
Finding the sweet spot: Sara Bleich’s talking points for halting obesity
Sara Bleich, professor of public health policy at the Harvard Chan School, was a 2015–2016 White House Fellow, where she served as a senior policy adviser to the U.S. Department of Agriculture (USDA) and to former first lady Michelle Obama’s Let’s Move! campaign. In a widely cited 2014 intervention in corner stores in low-income black neighborhoods of Baltimore (Bleich’s hometown), her team posted prominent signs near beverage displays. The signs listed calorie information, number of teaspoons of sugar, and number of minutes of running or miles of walking necessary to burn off calories in the beverage. The goal was to prompt teenagers to think twice about their purchases. Sugary drink sales dropped and the teens also started buying smaller bottles—effects that persisted after the signs were removed.
Below, Bleich discusses other fundamentals of effective public health communication.
1. Meet people where they are.
Typically, you change after a shock to your system. It could be watching someone in your family lose a leg because of diabetes. It could be learning the reality that if you gain weight, you’ll probably never lose it. Or that your weight is what makes you snore at night. In public health communication, you have to meet people where they are and relate to the values that matter to a person in that moment.
2. Find common ground with industry and policymakers.
How do you do obesity policy in a smart way? You find the sweet spot—not just what maximizes the public’s health but also what maximizes the interests of other parties. For example, if I said to a governor, “Look, if you pass this excise tax, you can generate revenue, reduce Medicaid spending, and improve students’ test scores while helping them lose weight,” he or she might think it’s worth pushing back against Pepsi and Coke.
3. Switch from gray to black and white.
Gray is the color of science. But when you’re talking to policymakers or advocates or people in the business sector, they don’t want nuance, they want black and white: Is something going to work or not? We need to take off our scientific hats and be precise and clear without confusing people.
4. Leverage corporations’ profit motive.
There are so many mixed messages about what is healthy and what is not. Public health made a huge mistake in deciding in the ’70s that consumers couldn’t differentiate between good fats and bad fats, so it declared all fat bad, and you had a generation of women eating Snackwell’s cookies. Then you had restaurant menus with Atkins-diet-only items. Now you’ve got people who are scared to have dinner with bread on the table. These huge pendulum swings stir up people’s crazy relationships with food. The point is that the food industry is very responsive—and if you can get consumers to demand healthier, lower-calorie food, that is probably one of the easiest ways to persuade industry to change, because it’s going to follow the dollars.
5. Don’t let idealism get in the way.
Let’s say that I was talking to the mayor of Boston, and I really wanted him to pass a sugary-beverage tax. But he says, “The best that I can do is a warning label.” You start there. Where public health often falls short is that it’s idealistic, and the perfect is the enemy of the good. Instead, carve your path and continue to chip away. The fact that Berkeley [California] passed a sugary beverage tax in 2014 paved the way for four other cities this past November, and for Seattle to propose a tax in February. That is not coincidental.
[/contentarea]
4.
Show them the money.
Obesity kills budgets. According to the Campaign to End Obesity, a collaboration of leaders from industry, academia, public health, and policymakers, annual U.S. health costs related to obesity approach $200 billion. In 2010, the nonpartisan Congressional Budget Office reported that nearly 20 percent of the rise in health care spending from 1987 to 2007 was linked to obesity. And the U.S. Centers for Disease Control and Prevention (CDC) found that full-time workers in the U.S. who are overweight or obese and have other chronic health conditions miss an estimated 450 million more days of work each year than do healthy employees—upward of $153 billion in lost productivity annually.
But making the money case for obesity prevention isn’t straightforward. For interventions targeting children and youth, only a small fraction of savings is captured in the first decade, since most serious health complications don’t emerge for many years. Long-term obesity prevention, in other words, doesn’t fit into political timetables for elected officials.
Yet lawmakers are keen to know how “best for the money” obesity-prevention programs can help them in the short run. Over the past two years, Harvard Chan’s Steve Gortmaker and his colleagues have been working with state health departments in Alaska, Mississippi, New Hampshire, Oklahoma, Washington, and West Virginia and with the city of Philadelphia and other locales, building cost-effectiveness models using local data for a wide variety of interventions—from improved early child care to healthy school environments to communitywide campaigns. “We collaborate with health departments and community stakeholders, provide them with the evidence base, help assess how much different options cost, model the results over a decade, and they pick what they want to work on. One constant that we’ve seen—and these are very different political environments—is a strong interest in cost-effectiveness,” he says.
[sidebar position=”right” offset=”true”]
[/sidebar]
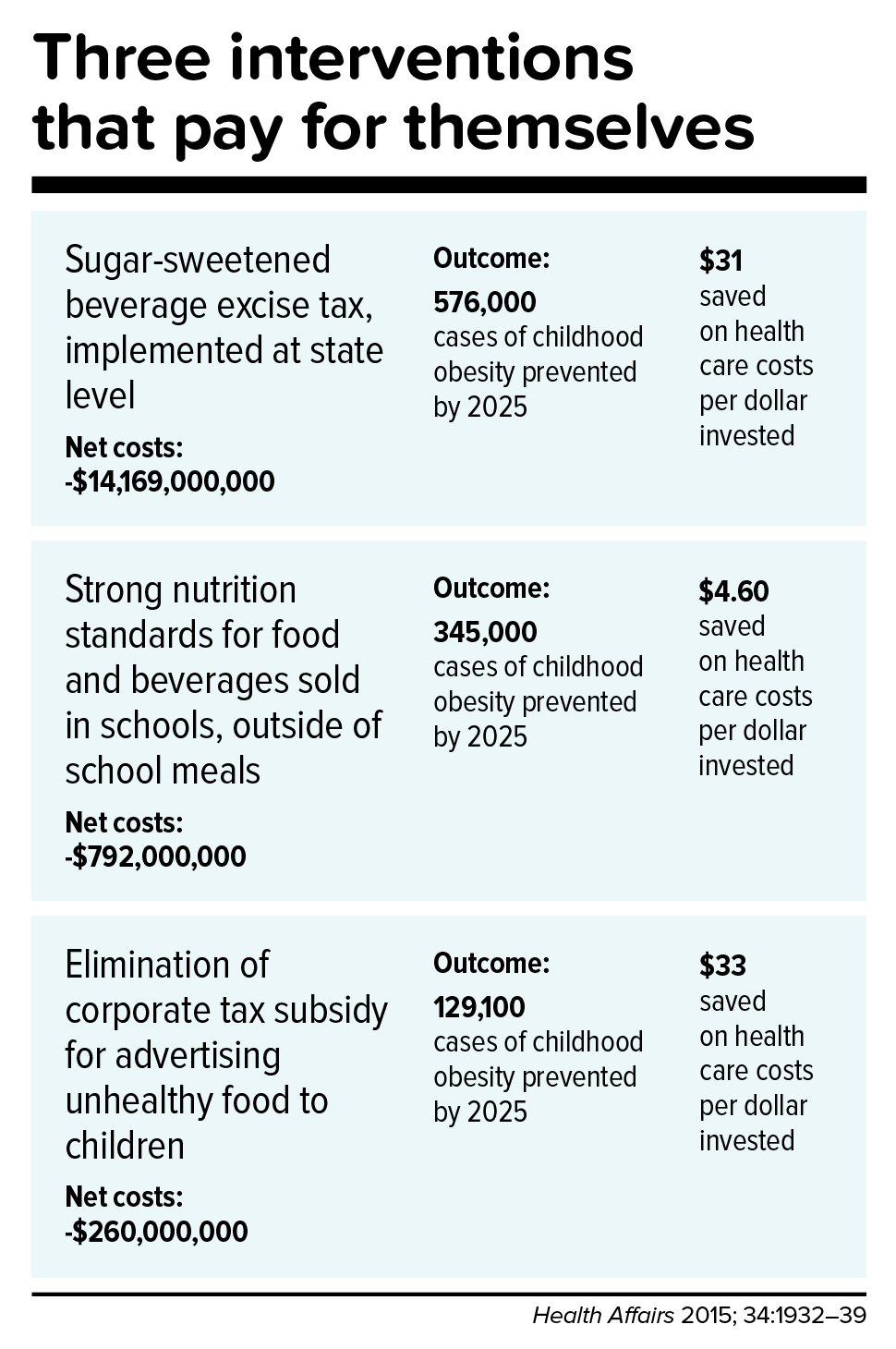
In a 2015 study in Health Affairs, Gortmaker and colleagues outlined three interventions that would more than pay for themselves: an excise tax on sugar-sweetened beverages implemented at the state level; elimination of the tax subsidy for advertising unhealthy food to children; and strong nutrition standards for food and drinks sold in schools outside of school meals. Implemented nationally, these interventions would prevent 576,000, 129,100, and 345,000 cases of childhood obesity, respectively, by 2025. The projected net savings to society in obesity-related health care costs for each dollar invested: $31, $33, and $4.60, respectively.
Gortmaker is one of the leaders of a collaborative modeling effort known as CHOICES—for Childhood Obesity Intervention Cost-Effectiveness Study—an acronym that seems a pointed rebuttal to the reflexive conservative argument that government regulation tramples individual choice. Having grown up not far from Des Plaines, Illinois, site of the first McDonald’s franchise in the country, he emphasizes to policymakers that at this late date, America cannot treat its way out of obesity, given current medical know-how. Only a thoroughgoing investment in prevention will turn the tide. “Clinical interventions produce too small an effect, with too small a population, and at high cost,” Gortmaker says. “The good news is that there are many cost-effective options to choose from.”
While Gortmaker underscores the importance of improving both food choices and options for physical activity, he has shown that upgrading the food environment offers much more benefit for the buck. This is in line with the gathering scientific consensus that what we eat plays a greater role in obesity than does sedentary lifestyle (although exercise protects against many of the metabolic consequences of excess weight). “The easiest way to explain it,” Gortmaker says, “is to talk about a sugary beverage—140 calories. You could quickly change a kid’s risk of excess energy balance by 140 calories a day just by switching from a sugary drink a day to water or sparkling water. But for a 10-year-old boy to burn an extra 140 calories, he’d have to replace an hour-and-a-half of sitting with an hour-and-a-half of walking.”
Small tweaks in adults’ diets can likewise make a big difference in short order. “With adults, health care costs rise rapidly with excess weight gain,” Gortmaker says. “If you can slow the onset of obesity, you slow the onset of diabetes, and potentially not only save health care costs but also boost people’s productivity in the workforce.”
One of Gortmaker’s most intriguing calculations spins off of the food industry’s estimated $633 million spent on television marketing aimed at kids. Currently, federal tax treatment of advertising as an ordinary business expense means that the government, in effect, subsidizes hawking of junk food to children. Gortmaker modeled a national intervention that would eliminate this subsidy of TV ads for nutritionally empty foods and beverages aimed at 2- to 19-year-olds. Drawing on well-delineated relationships between exposure to these advertisements and subsequent weight gain, he found that the intervention would save $260 million in downstream health care costs. Although the effect would probably be small at the individual level, it would be significant at the population level.
5.
Level the playing field through taxes and regulation.
When public health took on cigarette smoking, starting in the 1960s, it did so with robust policies banning television ads and other marketing, raising taxes to increase prices, making public places smoke-free, and offering people treatment such as the nicotine patch. In 1965, the smoking rate for U.S. adults was 42.2 percent; today, it is 16.8 percent.
Similarly, America reduced the rate of deaths caused by motor vehicle accidents—a 90 percent decrease over the 20th century, according to the CDC—with mandatory seat belt laws, safer car designs, stop signs, speed limits, rumble strips, and the stigmatization of drunk driving.
Change the product. Change the environment. Change the culture. That is also the policy recipe for stopping obesity.
Laws that make healthy behaviors easier are often followed by positive changes in those behaviors. And people who are trying to adopt healthy behaviors tend to support policies that make their personal aspirations achievable, which in turn nudges lawmakers to back the proposals.
One debate today revolves around whether recipients of federal Supplemental Nutrition Assistance Program (SNAP) benefits (formerly known as food stamps) should be restricted from buying sodas or junk food. The largest component of the USDA budget, SNAP feeds one in seven Americans. A USDA report, issued last November, found that the number-one purchase by SNAP households was sweetened beverages, a category that included soft drinks, fruit juices, energy drinks, and sweetened teas, accounting for nearly 10 percent of SNAP money spent on food. Is the USDA therefore underwriting the soda industry and planting the seeds for chronic disease that the government will pay to treat years down the line?
Eric Rimm, a professor in the Departments of Epidemiology and Nutrition at the Harvard Chan School, frames the issue differently. In a 2017 study in the American Journal of Preventive Medicine, he and his colleagues asked SNAP participants whether they would prefer the standard benefits package or a “SNAP-plus” that prohibited the purchase of sugary beverages but offered 50 percent more money for buying fruits and vegetables. Sixty-eight percent of the participants chose the healthy SNAP-plus option.
[sidebar position=”right” offset=”true”]
[/sidebar]
“A lot of work around SNAP policy is done by academics and politicians, without reaching out to the beneficiaries,” says Rimm. “We haven’t asked participants, ‘What’s your say in this? How can we make this program better for you?’” To be sure, SNAP is riddled with nutritional contradictions. Under current rules, for example, participants can use benefits to buy a 12-pack of Pepsi or a Snickers bar or a giant bag of Lay’s potato chips but not real food that happens to be heated, such as a package of rotisserie chicken. “This is the most vulnerable population in the country,” says Rimm. “We’re not listening well enough to our constituency.”
Other innovative fiscal levers to alter behavior could also drive down obesity. In 2014, a trio of strong voices on food industry practices—Dariush Mozaffarian, DrPH ’06, dean of Tufts University’s Friedman School of Nutrition Science and Policy and former associate professor of epidemiology at the Harvard Chan School; Kenneth Rogoff, professor of economics at Harvard; and David Ludwig, professor in the Department of Nutrition at Harvard Chan and a physician at Boston Children’s Hospital—broached the idea of a “meaningful” tax on nearly all packaged retail foods and many chain restaurants, with the proceeds used to pay for minimally processed foods and healthier meals for school kids. In essence, the tax externalizes the social costs of harmful individual behavior.
“We made a straightforward proposal to tax all processed foods and then use the income to subsidize whole foods in a short-term, revenue-neutral way,” explains Ludwig. “The power of this idea is that, since there is so much processed food consumption, even a modest tax—in the 10 to 15 percent range—is not going to greatly inflate the cost of these foods. Their price would increase moderately, but the proceeds would not disappear into government coffers. Instead, the revenue would make healthy foods affordable for virtually the entire population, and the benefits would be immediately evident. Yes, people will pay moderately more for their Coke or for their cinnamon bear claw but a lot less for nourishing, whole foods.”
[sidebar position=”right” offset=”true”]
[/sidebar]
Another suggestion comes from Sandro Galea, dean of the Boston University School of Public Health, and Abdulrahman M. El-Sayed, a public health physician and epidemiologist. In a 2015 issue of the American Journal of Public Health, they called for “calorie offsets,” similar to the carbon offsets used to mitigate environmental harm caused by the gas and oil industries. A “calorie offset” scheme could hand the food and beverage industries a chance at redemption by inviting them to invest in such undertakings as city farms, cooking classes for parents, healthy school cafeterias, and urban green spaces.
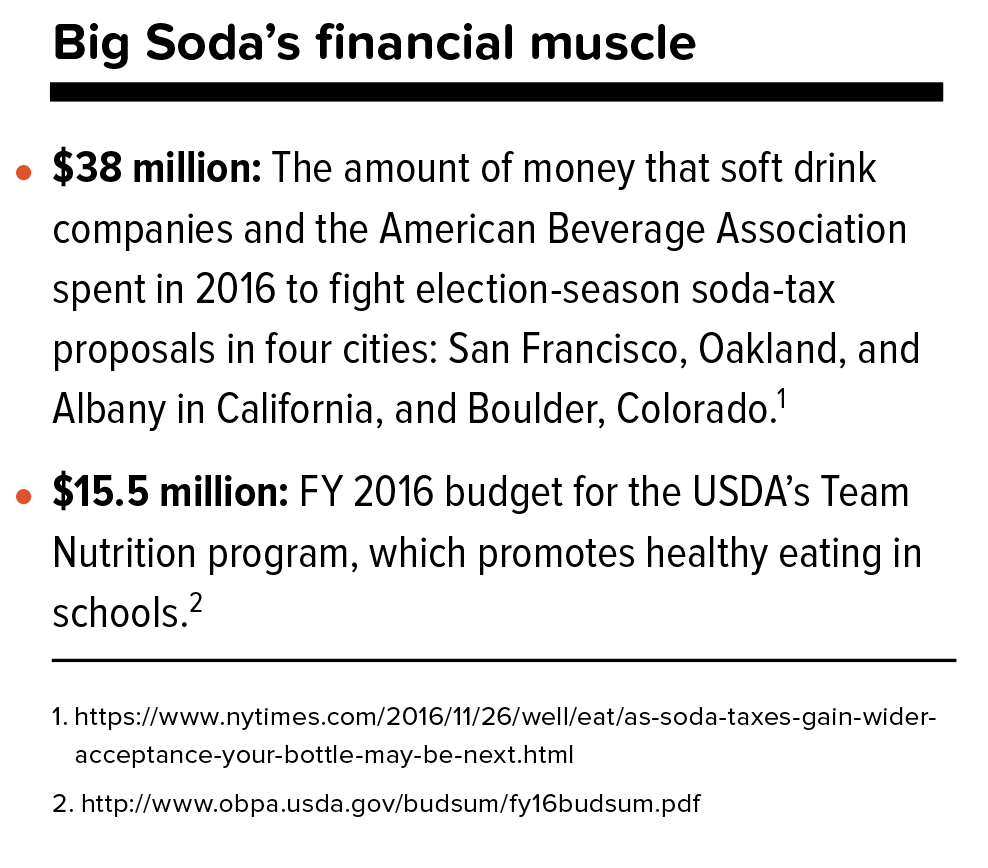
These ambitious proposals face almost impossibly high hurdles. Political battle lines typically pit public health against corporations, with Big Food casting doubt on solid nutrition science, deeming government regulation a threat to free choice, and making self-policing pledges that it has never kept. On the website for the Americans for Food and Beverage Choice, a group spearheaded by the American Beverage Association, is the admonition: “[W]hether it’s at a restaurant or in a grocery store, it’s never the government’s job to decide what you choose to eat and drink.”
Yet surprisingly, many public health professionals are convinced that the only way to stop obesity is to make common cause with the food industry. “This isn’t like tobacco, where it’s a fight to the death. We need the food industry to make healthier food and to make a profit,” says Mozaffarian. “The food industry is much more diverse and heterogeneous than tobacco or even cars. As long as we can help them—through carrots and sticks, tax incentives and disincentives—to move towards healthier products, then they are part of the solution. But we have to be vigilant, because they use a lot of the same tactics that tobacco did.”
6.
Sow what we want to reap.
Americans overeat what our farmers overproduce.
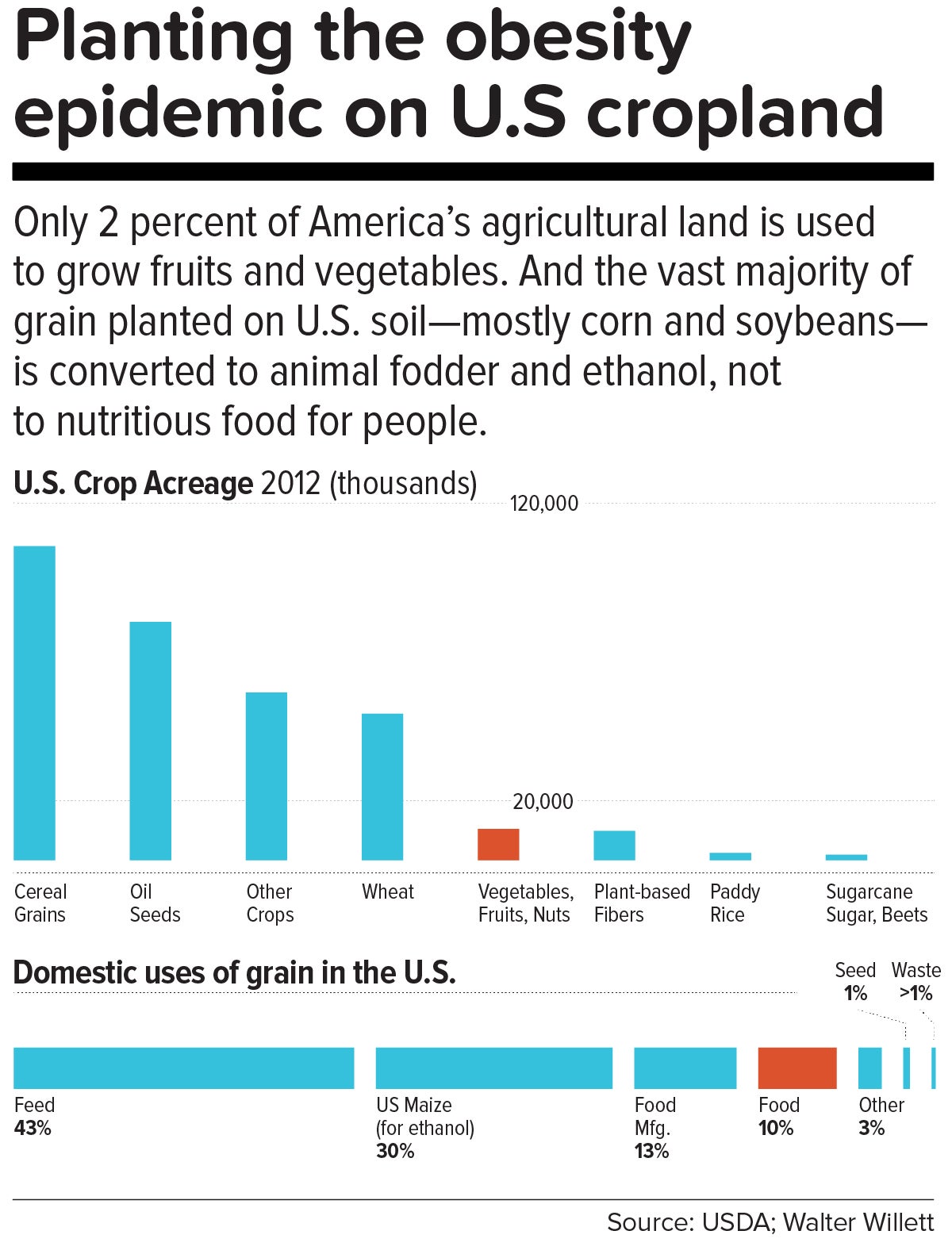
“The U.S. food system is egregiously terrible for human and planetary health,” says Walter Willett. It’s so terrible, Willett made a pie chart of American grain production consumed domestically. It shows that most of the country’s agricultural land goes to the two giant commodity crops: corn and soy. Most of those crops, in turn, go to animal fodder and ethanol, and are also heavily used in processed snack foods. Today, only about 10 percent of grain grown in the U.S. for domestic use is eaten directly by human beings. According to a 2013 report from the Union of Concerned Scientists, only 2 percent of U.S. farmland is used to grow fruits and vegetables, while 59 percent is devoted to commodity crops.

Historically, those skewed proportions made sense. Federal food policies, drafted with the goal of alleviating hunger, preferentially subsidize corn and soy production. And whereas corn or soybeans could be shipped for days on a train, fruits and vegetables had to be grown closer to cities by truck farmers so the produce wouldn’t spoil. But those long-ago constraints don’t explain today’s upside-down agricultural priorities.
[sidebar class=”ob-graphic” position=”right” offset=”true”]
[/sidebar]
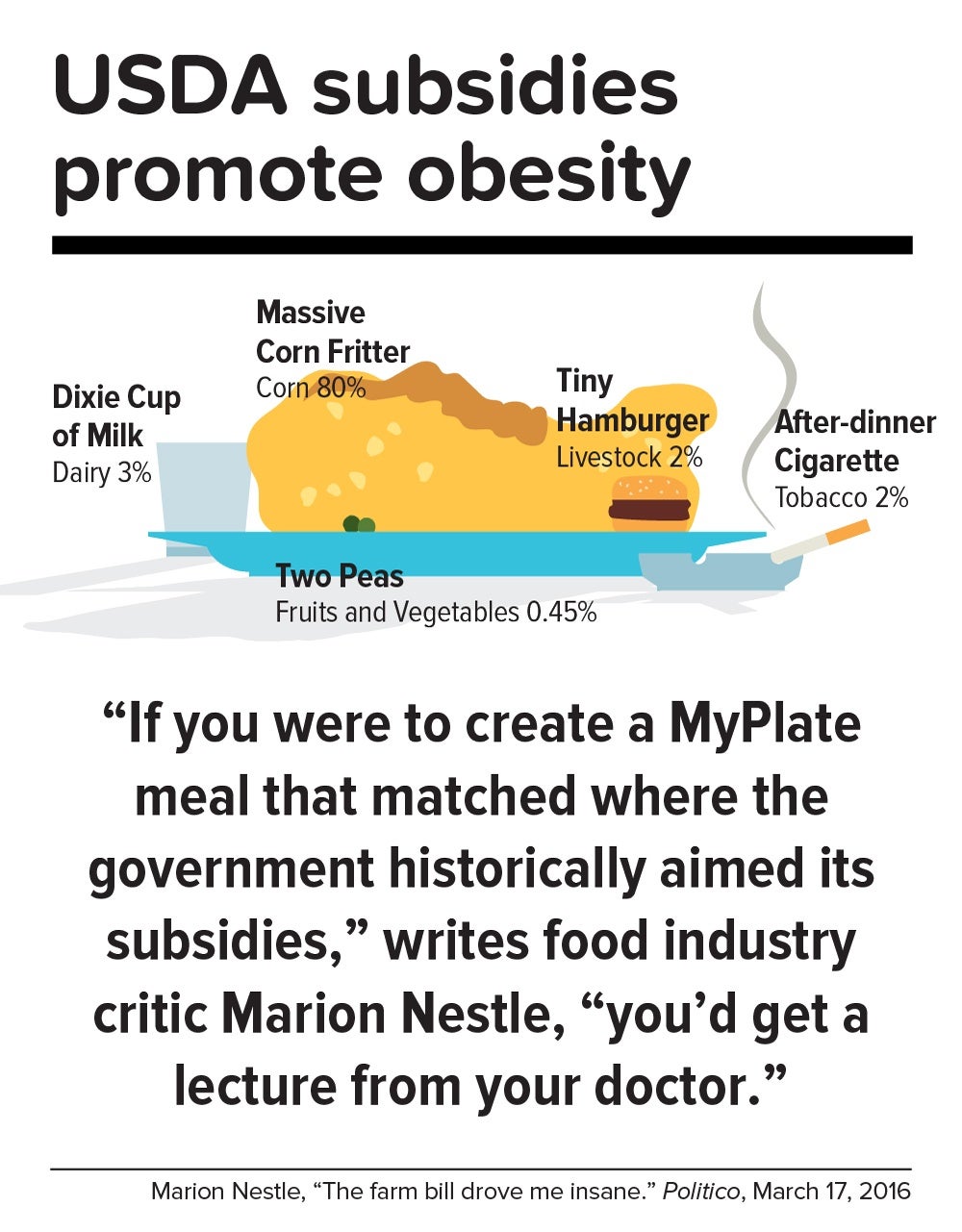
In a now-classic 2016 Politico article titled “The farm bill drove me insane,” Marion Nestle illustrated the irrational gap between what the government recommends we eat and what it subsidizes: “If you were to create a MyPlate meal that matched where the government historically aimed its subsidies, you’d get a lecture from your doctor. More than three-quarters of your plate would be taken up by a massive corn fritter (80 percent of benefits go to corn, grains and soy oil). You’d have a Dixie cup of milk (dairy gets 3 percent), a hamburger the size of a half dollar (livestock: 2 percent), two peas (fruits and vegetables: 0.45 percent) and an after-dinner cigarette (tobacco: 2 percent). Oh, and a really big linen napkin (cotton: 13 percent) to dab your lips.”
In this sense, the USDA marginalizes human health. Many of the foods that nutritionists agree are best for us—notably, fruits, vegetables, and tree nuts—fall under the bureaucratic rubric “specialty crops,” a category that also includes “dried fruits, horticulture, and nursery crops (including floriculture).” Farm bills, which get passed every five years or so, fortify the status quo. The 2014 Farm Bill, for example, provided $73 million for the Specialty Crop Block Grant Program in 2017, out of a total of about $25 billion for the USDA’s discretionary budget. (The next Farm Bill, now under debate, will be coming out in 2018.)
By contrast, a truly anti-obesigenic agricultural system would stimulate USDA support for crop diversity—through technical assistance, research, agricultural training programs, and financial aid for farmers who are newly planting or transitioning their land into produce. It would also enable farmers, most of whom survive on razor-thin profit margins, to make a decent living.
7.
Mobilize.
In the early 1970s, Finland’s death rate from coronary heart disease was the highest in the world, and in the eastern region of North Karelia—a pristine, sparsely populated frontier landscape of forest and lakes—the rate was 40 percent worse than the national average. Every family saw physically active men, loggers and farmers who were strong and lean, dying in their prime.
Thus was born the North Karelia Project, which became a model worldwide for saving lives by transforming lifestyles. The project was launched in 1972 and officially ended 25 years later. While its initial goal was to reduce smoking and saturated fat in the diet, it later resolved to increase fruit and vegetable consumption.
The North Karelia Project fulfilled all of these ambitions. When it started, for example, 86 percent of men and 82 percent of women smeared butter on their bread; by the early 2000s, only 10 percent of men and 4 percent of women so indulged. Use of vegetable oil for cooking jumped from virtually zero in 1970 to 50 percent in 2009. Fruit and vegetables, once rare visitors to the dinner plate, became regulars. Over the project’s official quarter-century existence, coronary heart disease deaths in working-age North Karelian men fell 82 percent, and life expectancy rose seven years.
The secret of North Karelia’s success was an all-out philosophy. Team members spent innumerable hours meeting with residents and assuring them that they had the power to improve their own health. The volunteers enlisted the assistance of an influential women’s group, farmers’ unions, homemakers’ organizations, hunting clubs, and church congregations. They redesigned food labels and upgraded health services. Towns competed in cholesterol-cutting contests. The national government passed sweeping legislation (including a total ban on tobacco advertising). Dairy subsidies were thrown out. Farmers were given strong incentives to produce low-fat milk, or to get paid for meat and dairy products based not on high-fat but on high-protein content. And the newly established East Finland Berry and Vegetable Project helped locals switch from dairy farming—which had made up more than two-thirds of agriculture in the region—to cultivation of cold-hardy currants, gooseberries, and strawberries, as well as rapeseed for heart-healthy canola oil.
“A mass epidemic calls for mass action,” says the project’s director, Pekka Puska, “and the changing of lifestyles can only succeed through community action. In this case, the people pulled the government—the government didn’t pull the people.”
Could the United States in 2017 learn from North Karelia’s 1970s grand experiment?
“Americans didn’t become an obese nation overnight. It took a long time—several decades, the same timeline as in individuals,” notes Frank Hu. “What were we doing over the past 20 years or 30 years, before we crossed this threshold? We haven’t asked these questions. We haven’t done this kind of soul-searching, as individuals or society as a whole.”
Today, Americans may finally be willing to take a hard look at how food figures in their lives. In a July 2015 Gallup phone poll of Americans 18 and older, 61 percent said they actively try to avoid regular soda (the figure was 41 percent in 2002); 50 percent try to avoid sugar; and 93 percent try to eat vegetables (but only 57.7 percent in 2013 reported they ate five or more servings of fruits and vegetables at least four days of the previous week).
[contentarea class=”obesity-section-2″]
A playbook for healthy-food activists
How can advocates for a wholesome food environment transform the American eating landscape? By telling their stories, turning time into power, and mobilizing action, says veteran organizer Marshall Ganz, senior lecturer in public policy at the Harvard Kennedy School.
Ganz teaches people how to convert community resources into a force for social change. His approach is grounded in what he terms “public narrative: a story of self, a story of us, and a story of now.” A “story of self” draws on moments of one’s own life experience, which enables others to “get” why one has been called to act. A “story of us” invokes values rooted in shared experience. A “story of now” frames the present as a time of challenge, a choice to be made, and a source of hope.
In the case of the obesity epidemic, a story of self could describe one’s own experience as a young child struggling with overweight or growing up in a fresh-food desert—someone without much chance against a fattening food environment—and where one found the hope to change. “It’s not making the case in terms of data. It’s making the case experientially,” says Ganz. “Unless there’s a human connection, it’s hard for people to engage with the challenge. Values are emotional in content—they are not simply ideas.”
Ganz’s approach bridges the moral ground of experience with action. That could mean firmly asking your city councilors to serve healthy food at official events, shopping only at supermarkets that offer healthy provisions, asking the medical staff to actively support a campaign to have hospitals sell fresh fruit in their cafeterias, leveraging social media to amplify all these demands—and training people in the practice of organizing.
Above all, public narrative rests on sharing stories of hope as well as hurt. “The definition of hope that I like comes from Maimonides, who said that hope is belief in the plausibility of the possible, as opposed to the necessity of the probable,” says Ganz. “To be a realist is to recognize that it is probable Goliath will always win—but that, sometimes, David does.”
[/contentarea]
Individual resolve, of course, counts for little in problems as big as the obesity epidemic. Most successes in public health bank on collective action to support personal responsibility while fighting discrimination against an epidemic’s victims. [To learn more about the perils of stigma against people with obesity, read “The Scarlet F.”]
Yet many of public health’s legendary successes also took what seems like an agonizingly long time to work. Do we have that luxury?
“Right now, healthy eating in America is like swimming upstream. If you are a strong swimmer and in good shape, you can swim for a little while, but eventually you’re going to get tired and start floating back down,” says Margo Wootan, SD ’93, director of nutrition policy for the Center for Science in the Public Interest. “If you’re distracted for a second—your kid tugs on your pant leg, you had a bad day, you’re tired, you’re worried about paying your bills—the default options push you toward eating too much of the wrong kinds of food.”
But Wootan has not lowered her sights. “What we need is mobilization,” she says. “Mobilize the public to address nutrition and obesity as societal problems—recognizing that each of us makes individual choices throughout the day, but that right now the environment is stacked against us. If we don’t change that, stopping obesity will be impossible.”
The passing of power to younger generations may aid the cause. Millennials are more inclined to view food not merely as nutrition but also as narrative—a trend that leaves Duke University’s Kelly Brownell optimistic. “Younger people have been raised to care about the story of their food. Their interest is in where it came from, who grew it, whether it contributes to sustainable agriculture, its carbon footprint, and other factors. The previous generation paid attention to narrower issues, such as hunger or obesity. The Millennials are attuned to the concept of food systems.”
We are at a public health inflection point. Forty years from now, when we gaze at the high-resolution digital color photos from our own era, what will we think? Will we realize that we failed to address the obesity epidemic, or will we know that we acted wisely?
The question brings us back to the 1970s, and to Pekka Puska, the physician who directed the North Karelia Project during its quarter-century existence. Puska, now 71, was all of 27 and burning with big ideas when he signed up to lead the audacious effort. He knows the promise and the perils of idealism. “Changing the world may have been utopic,” he says, “but changing public health was possible.”