Why ‘good’ cholesterol may not always be good

February 16, 2022 – For decades, it’s been known that, when it comes to heart disease risk, there’s a difference between so-called “bad cholesterol”—also known as low-density lipoprotein or LDL, which can clog up the artery walls—and “good cholesterol,” known as high-density lipoprotein or HDL, which helps clear cholesterol out of the system. Recently, drugs have been developed that increase the amount of HDL in the blood, but disappointingly failed to reduce the risk of cardiovascular disease and were never brought to market. A December paper co-authored by Harvard T.H. Chan School of Public Health researchers Jeremy Furtado, Frank Sacks, and colleagues, helps explain why the drugs didn’t work. In this Big 3 Q&A, Furtado elaborates on their findings.
Q: People call HDL “good cholesterol” because it helps remove cholesterol out of the body—but you seem to say that’s not always the case. Why is that moniker not entirely accurate?
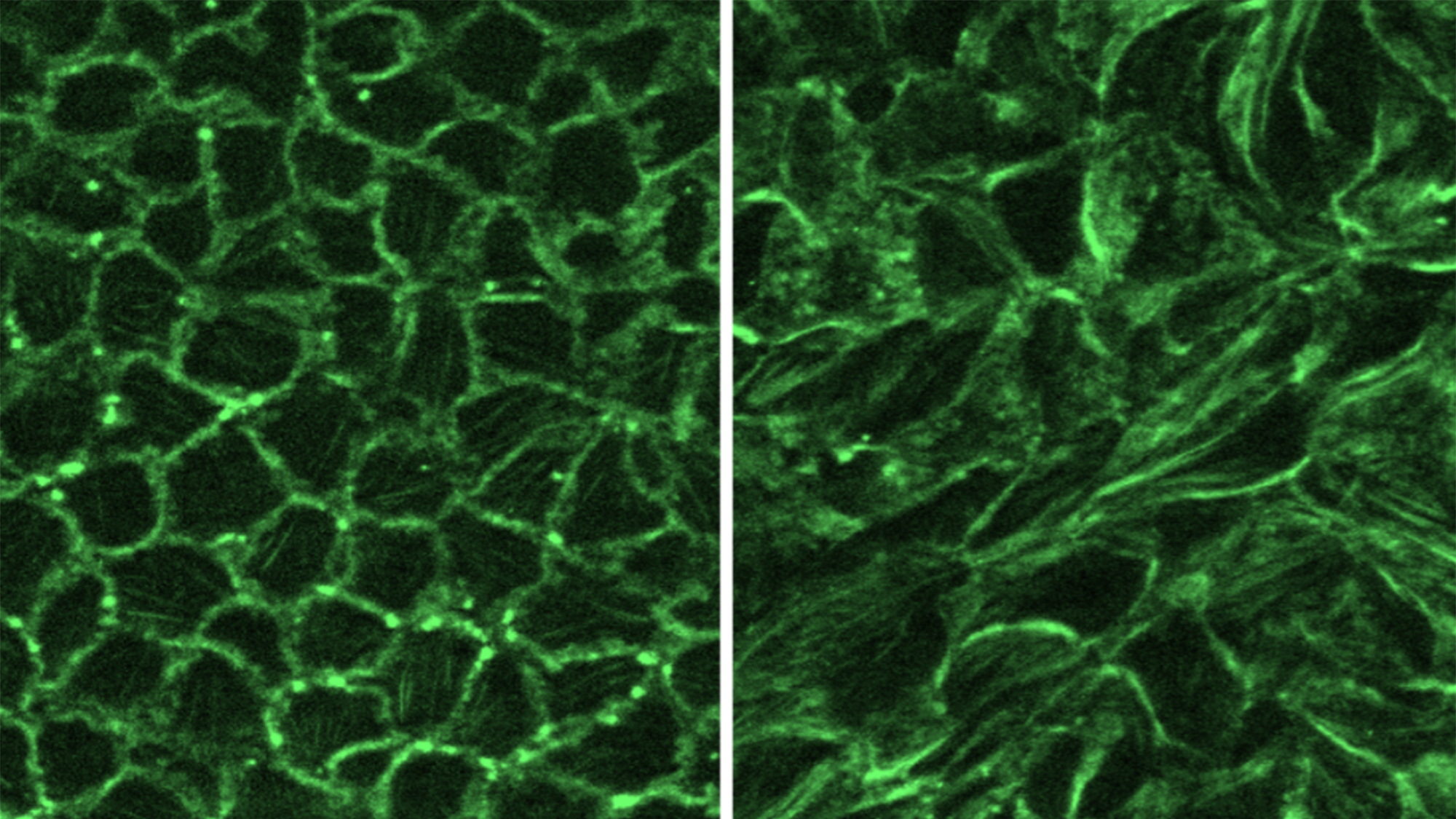
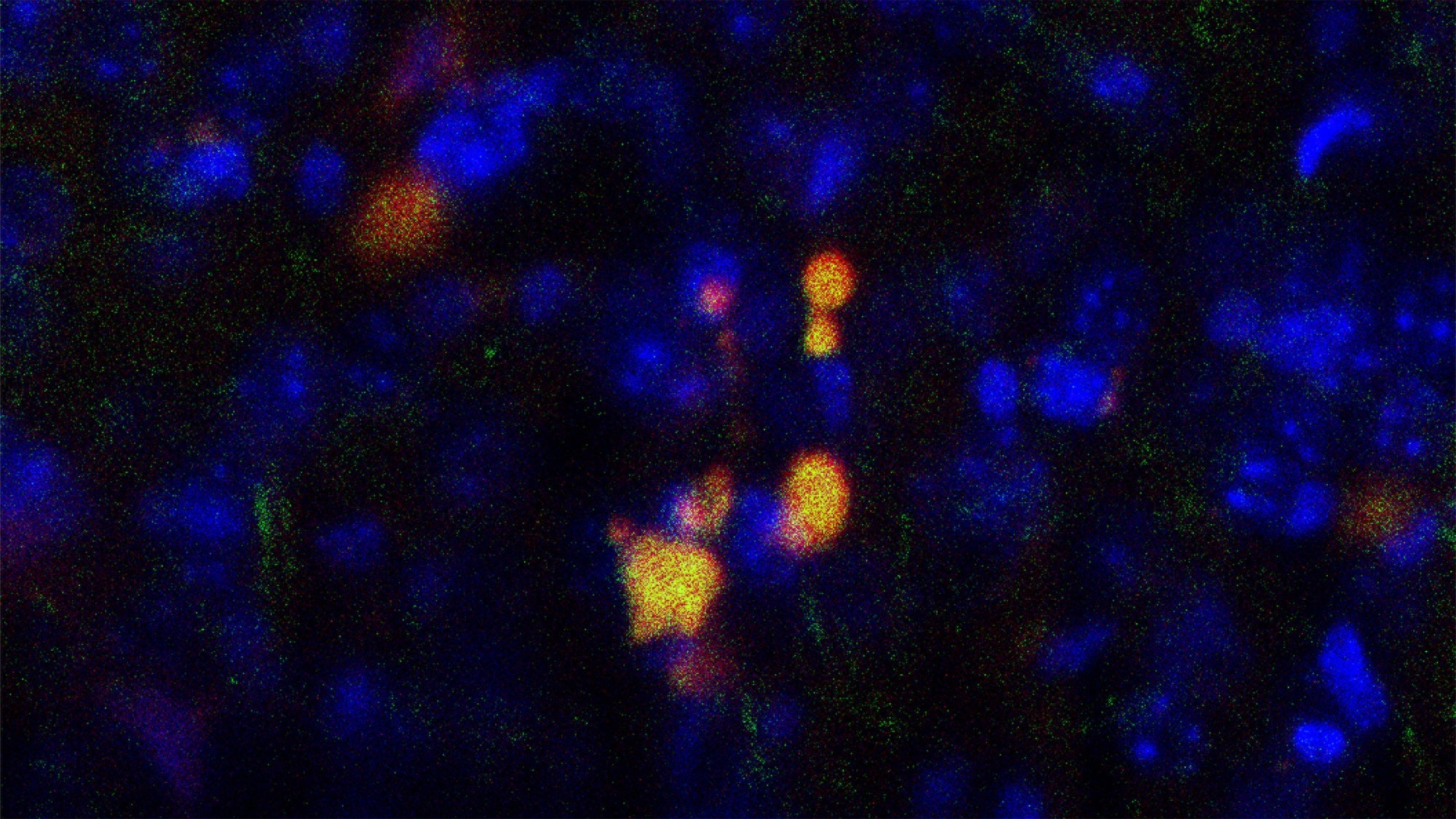
A: In the middle of the last century, total cholesterol was an important biomarker used to assess heart disease risk. Then, in the 1970s and 1980s, researchers discovered that total cholesterol is actually made up of two very different systems, the LDL and HDL, with opposing relationships with heart disease risk. Generally speaking, cholesterol in LDL is linked to increased risk while cholesterol in HDL is associated with protection against heart disease. More recently, our group here at Harvard Chan School found that within HDL there are different subspecies that have different types of proteins on their surfaces that make them function differently from each other in the body. Given these functional differences, why should we expect that they are all protective or operate the same way? Recently, we’ve been studying 16 out of the potentially 200 or so different protein-defined HDL subspecies and found that while some are associated with a reduced risk of cardiovascular disease as you’d expect, some show no association or are even associated with increased risk. In particular, we found that HDL that contains a protein called apolipoprotein C3 (apoC3) is associated with a higher risk of cardiovascular disease, including stroke and heart attack, and type 2 diabetes. We also found that HDL that contains Complement C3 or alpha-2-Macroglobulin (α2M) is also associated with higher risk. HDLs that lack these proteins are more protective than total HDL. Conversely, HDL that contains apolipoprotein E (apoE) or apolipoprotein C1 (apoC1) is more protective against heart disease.
Q: In your study, you looked at a class of drugs called CETP inhibitors, specifically evacetrapib (Eli Lilly) and torcetrapib (Pfizer). What happened to cholesterol levels and cardiovascular disease when people took these medications?
A: CETP is a protein that moves cholesterol from HDL into LDL, so these CETP inhibitor drugs increase HDL cholesterol. While they succeeded in this, phase three clinical trials showed that there wasn’t a significant decrease in cardiovascular disease outcomes, including heart attack. So CETP inhibition wasn’t having the intended effect of reducing mortality and heart disease. The failure of these trials and trials like them, coupled with other studies that showed that naturally occurring genetic mutations that resulted in high HDL cholesterol also did not confer any protection against heart disease, implied to some that HDL was not truly an actor in the disease. Our hypothesis was that maybe the different protein-defined subspecies have different relationships with disease, some bad and some good, and perhaps these drugs didn’t work because even though they increased overall HDL cholesterol, it was the bad kinds that went up. And, in fact, we found the types of HDL that went up the most were the ones that were the worst, including those that contained apoC3.
Q: What are the health implications of these findings? Is there a way that pharma companies could retool these drugs, or other things that people can do to increase their good good cholesterol?
A: One of the most important things to come out of this study is to underscore the need to learn more about HDL subspecies to find out what functions these proteins perform. HDL isn’t just a cholesterol transporter. It also has anti-inflammatory, antioxidant, immunological, and other actions that affect disease risk. We need to find out which HDL subspecies are protective and which ones are detrimental. Once we know that, we can work to produce therapies that will target increases of the good types of HDL or reductions of the bad. And it’s not just drug therapies. Our group will soon publish new research on the effects of healthy diets associated with reduced risk of heart disease that increase HDL cholesterol, and do so by increasing the good HDL subspecies and not the bad. Stay tuned!