Coronavirus (COVID-19): Press Conference with Barry Bloom, 08/11/20
You’re listening to a press conference from the Harvard T.H. Chan School of Public Health with Barry Bloom, the Joan L. and Julius H. Jacobson Research Professor of Public Health. This call was recorded at 11:30 a.m. Eastern Time on Tuesday, August 11th.
Transcript
MODERATOR: Doctor, do you have any opening remarks, perhaps?
BARRY BLOOM: I’d like to say that the more we go along, the less certainty I seem to have on all kinds of subjects. The Russians have made what they claim is the first vaccine, but we’re uncertain how many people have ever received that, whether they’ve been through trials, what the data are. There’s uncertainty as to whether children get serious infection, have high levels of virus, transmit to family members, transmit to others, and yet decisions have to be made on all of that stuff. So I caution whatever I say has a degree of uncertainty that I will try to be honest about.
MODERATOR: All right. Looks like our first question.
Q: Hi. Thanks so much for doing this yet again. I appreciate it. And I have pretty much as many questions as you do, so I could go on for most of this time. But maybe start by by amplifying one of the things you said. And then I have a different question, but talk a little bit, if you would, about what you think of this Russian vaccine. Do you think it’s possibly safe? What do you think people in Russia should be doing about it?
BARRY BLOOM: The vaccine is kind of interesting to me because apparently we only learn from press releases, there are no published data of which I’m aware, that it’s a mixture of two adenovirus strains, both of which have been used in vaccines in other countries. So it’s a mix of adeno-5 and adeno-26. The Chinese have already tested adeno-5 recombinant with spike protein, reported that they thought it was safe and made antibodies. But the problem with that, adeno-5 is an awful lot of people have antibodies already to adeno-5, simply because it’s a common respiratory virus. Even in the Chinese paper with that strain, they indicated that those that had prior antibodies had a poor antibody response.
Adeno-26 is the basis of the other Russian vaccine, but it is also the Johnson and Johnson vaccine, again with the spike protein heavily organized by Dan Barouch at Beth Israel Deaconess in Boston. Adeno 26 is again a respiratory common virus, but very much less common in humans than many of the other strains and was picked primarily, I presume, so that there wouldn’t be a lot of antibody against the virus that would diminish the effect of the vaccine. And that obviously leads to why the Brits chose a chimpanzee adenovirus. The obvious reason is that humans have no experience with that. The Chinese are developing one from a chimpanzee adenovirus. So in the Russian case, the adeno-5, I think is not a terrific advantage. They did claim to have experience with using these strains for making an Ebola vaccine. So this isn’t their first start.
The real concern is we know nothing about phase one studies, how many people. We know nothing about phase two studies, how many people. The implications of the Wall Street Journal today is they can register the vaccine in Russia without having done a phase three trial for efficacy and safety. No one can believe that they could get 30,000 people in two months to have run a phase three trial. So it’s very hard to take this seriously unless they have used it in massive numbers of people and actually have the data. The press releases from Russia said it’s been tested in the military. I’d love to know if they were volunteers or this was an assignment. So we really don’t know much about either the efficacy and safety of the vaccine, or under the conditions in which it was registered in the UK.
WHO has reported they have contacted WHO for discussions about the issue of pre-qualification. Nobody and many middle income and low income countries will purchase a vaccine unless it’s been pre-approved or pre qualified by WHO, and those standards are pretty rigorous. Maybe a little less so and less bureaucratic, believe it or not, than FDA. But nonetheless, that’s the standard in which most and international drugs and vaccines are allowed to be so easily in low and middle income countries. So that’s about what I know about the Russian vaccine. There’s no reason based on what we know about the adeno-26 in monkeys, the chimp adenovirus of the UK, that it shouldn’t work and at least produce antibodies. And in both of those cases, the antibodies in the phase two trials were comparable to or exceeded the level of neutralizing antibodies found in convalescent patients who had recovered from coronavirus-19 disease.
Q: So did they win the battle or are we still fighting the war here?
BARRY BLOOM: You know, I just think the whole war and the battle is really ridiculous in terms of the race for a vaccine, I would say. It’s unclear what it means to win the race, since nobody has the capacity to produce all the vaccines required to protect the whole world, if there’s seven point six billion people in the world and you say 60 percent have to be immunized to provide community protection or commonly known as, inappropriately, herd immunity. Nobody can make that many billions of vaccine. So the U.S. is contracting multiple suppliers, as are the Europeans, to be able to get 100 million doses. We have 300 million that would be necessary, and two to three hundred million in the states alone. So the more the merrier in terms of trying to get a selection of the best possible vaccines. Those that have the highest level and the more enduring production of whatever the immune responses are that are protective, and could get it from as many sources that they are up as possible. One knows nothing about the scale that the Russians could do. I would say in an earlier life I’d been involved with DARPA and and with the National Academy and Biosecurity. Gamaleya is one of the really good research institutes in Russia. Russia had been at the forefront of bio terrorism research, way exceeding our capacity, and then the United States foresaw the use of biological weapons and only did defense work. There’s some good technology, background and science and technology in the Soviet Union and Russia now. So I have no reason to believe that they can’t do it right. It’d be nice if they allowed some transparency in what they’ve done.
Q: I’ll ask more later after other people are gone. Thanks.
MODERATOR: Next question.
Q: Thank you, Nicole. And thank you, Dr. Bloom, for doing this, I appreciate it. Doctor, let me ask you a question about testing. Testing, especially turnaround testing, is becoming more and more in demand as more states like Massachusetts require people traveling back from somewhere that had an outbreak to either quarantine 14 days or give us a test three days old. How quick are the quick tests that we’re seeing turned around? And if they are accurate, why aren’t they being used more?
BARRY BLOOM: What’s the second part of the question, why isn’t what being used more?
Q: There are quick tests going on.
BARRY BLOOM: Yeah. So we have a wonderful scientists at the school who does these press conferences often, Michael Mina, and he’s been heavily involved in Boston in setting up massive testing at the Broad Institute for not only the Boston area, but many universities in the Commonwealth. And the case is as follows. And it’s a really challenging ethical problem, at least from my perspective, and I think many. The gold standard that we’ve known for a long time is PCR testing, looking for fragments of RNA in the upper respiratory tract, hopefully reflecting something in the lower respiratory tract for evidence and footprints of the virus. The test, as it’s done, doesn’t tell you whether the virus is dead or alive, whether it’s capable of transmission or not. It tells you that someone has the virus. It’s pretty sensitive and it can be made semi quantitative.
The problem is that we have many, many too few tests, that they have to be done with expensive machinery, the tests are expensive in themselves. You have to go somewhere to be tested. They are limited often to people that have symptoms. Consequently, we have relatively little data on zero to nine or ten age children. It’s as good as we can do in terms of specificity and sensitivity. But given the number of cases that we have in this country, indeed, we are overwhelmed and unable to be able to do the number of tests that we need by the standard PCR test. And even with that test, where if you assume that for every positive individual, there will be on the order of 10 contacts, we’re simply overwhelmed in the ability to track down every contact, let alone have people answer the telephone and agree to isolate themselves. And it’s the isolation, not the test, which stops the chains of transmission, amidst the public health intervention. So Mike and a number of his colleagues and certainly a number of leaders in the biotechnology business, say this is not working and it’s not going to work unless the numbers of cases are low enough, that it’s pretty easy for anybody who wants or needs to get a test.
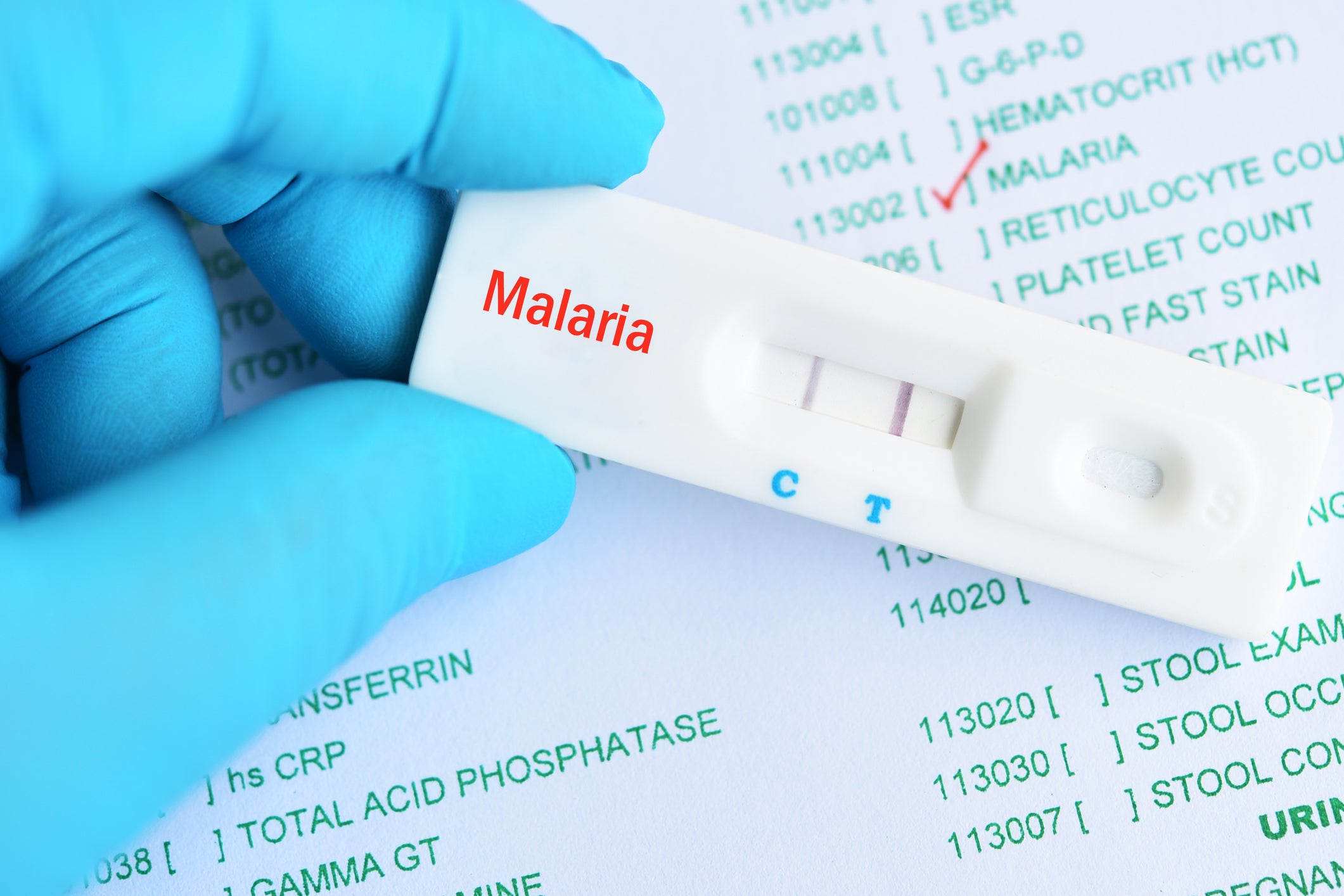
There are two kinds of rapid tests, and the one that is now currently become available recently are tests for antigen. It’s simply a paper strip with an imprint of a very good monoclonal antibody, often not to the spike protein, but to the major nucleocapsid antigen, that will tell you whether in a nasal sample there is antigen from the virus. What the PCR test can do is take a small amount of DNA and with reverse transcriptase make many, many, many, many copies. In fact, the quantitative aspect tells you how many copies you have to make to get a positive signal. And that’s a measure of how much RNA there was in the sample. It amplifies and the investigator can amplify it, even with a very small amount of virus. That’s why it’s so sensitive. You can’t do that with antigen. You have a certain amount of antigen. You have a certain amount of antibody. Either it’s enough to give a color test or a line on a paper, or it is not. Estimates of some of the more quantitative or commercial tests that are very good, which suggests to the effect of about maybe 50 percent relative to PCR. They’re all calibrated against PCR. And what Michael Mina’s position would be, look, we don’t have enough tests to care for everybody and to find everybody. Wouldn’t it be terrific if we could have at the point of care at a doctor’s office, at a pharmacist, and ultimately a pregnancy-like test that you could do in the household where everybody could test themselves?
And one of the things about the PCR test in the real world is, a test on one day doesn’t mean that two days later, a student coming back to college is not going to be positive. And it really isn’t practical unless you’re very wealthy in a college, to test people every other day by the PCR test. That’s going to be very difficult, certainly for schools to do. So a simple, cheap test, even if not effective and efficacious as PCR, would enable mass screening on a regular basis. That would have a huge public health impact but not be ideal for diagnosing. It will miss some cases that have low levels of virus that it simply can’t detect. And Michael’s argument is, if those people with very low levels have low levels, they’re unlikely to be big transmitters. If you can test every two days or three days or once a week, if they’re preclinical, two days later, they will have more virus and you’ll know that they’re positive. And then you would go to a place to get a PCR test done. So it’s a difference between using the tests for diagnosis to be precise and the tests at the public health level that can be used repeatedly to indicate sources of infection. Whether in a classroom, in a school, there are five or six kids that turn positive with a very cheap, very rapid test that might cost on the order of one to three dollars as opposed to one hundred dollars a pop. That’s the argument. And the concern is the gold standard is how the FDA sets its standards and requires other tests to be comparable to the gold standard tests. And that’s going to require, I think, rethinking by the FDA, redefining the standards for tests versus those that are used for diagnosis and those that have very powerful public health implications are not perfect for diagnosis, but are an awful lot more practical. And that’s a decision that I know has been raised with the FDA and no decision has been forthcoming.
There’s a third level of quick tests of which I am quite enthusiastic, which you’re using CRISPR by the two major developed by biotech company, spun off by the two famous CRISPR laboratories in San Francisco and the brood. And they’re very, very clever. And again, they can be done on paper. They can provide very rapid results in principle. None of them is commercially available, to my knowledge. None of them is likely to be as sensitive as the PCR test. We don’t know, or at least I don’t know, and haven’t seen written up how close they come in sensitivity. But they could be done again every day, every two days, every three days for a buck, the three bucks a piece. And from my perspective, don’t require a lot of equipment can be very simple and can be used for countries low and middle income countries all around the world, which is a desperate need since so many of those countries simply cannot do and afford to do the PCR test.
Q: Thank you, doctor.
MODERATOR: Next question.
Q: Hi, can you hear me?
BARRY BLOOM: Yes, I can.
Q: Dr. Bloom, thanks for taking the time. You covered a lot of kind of what I was gonna get into. But here in Texas, and across southern states, you’ve started to see a drop in testing as our surges have ebbed. And here in Texas, what’s been interesting in the last week is our testing has just kind of fallen off a cliff. We’ve doing half the rolling averages, roughly half of what it was in late July. The drop seems to be outpacing our drop in cases. You’ve seen that in our positivity rate increasing recently. I just wondered, it seems to be that a lot of this is demand driven. Local officials say fewer people are seeking out tests. And so I’m just wondering how a state like Texas or any state that has kind of gone through the biggest part of its surges and are now coming on the back side of that can keep the momentum of people getting tested and making sure that we’re not losing that speed that we’ve picked up as we started surveying the cases.
BARRY BLOOM: Thanks for the question, and it’s one of the many answers that I do not have that will be useful, I’m afraid. What we’ve been seeing is a degree at every level of COVID fatigue that I don’t think any people or many people in the medical business had anticipated. In the beginning, we were dealing with people that were sick, that were hospitalized. And this you remember, testing was restricted for those that had the greatest need, those that were or were sick. In many respects, as the cases fall, the public health need is to find out who are the transmitters, which are likely to be younger people, many of them asymptomatic. And there is no demand of those people, as there would be for people who have sickness or think they have COVID, to get tested. And hence, with fewer people hospitalized as those numbers go down and hopefully fewer deaths, which will follow the incentive for ordinary people to get tested, it diminishes. We’ve been at this for seven months and there’s a great deal of fatigue.
The only thing that I can say is I think it’s going to be very hard without enormously coherent leadership in the state, real PR, and incentives to people, particularly for checking on school kids as we go back to school. I think it’s going to be hard everywhere to persuade people to keep getting tested. And that’s another argument why we need a less sensitive perhaps, but a test that can be done by people, hopefully as a do it yourself test, as some of these are seeking to do. That would be a game changer from the point of view of public health. People wouldn’t have to take the trouble to go to a hospital or a clinic or whatever they could be to do it or in their household or go to the local pharmacy. And for a small amount of money, they would know whether they or their children are infected. I think we’re in an interim phase. I don’t expect any of the tests that I’ve talked about that are do it yourself, or home tests, or allowed to be done in pharmacies to be approved till the end of the summer. So we’re in a lag phase where I think we’re going to see just what you say, testing fatigue and then pessimism. If they keep hearing on the news, we’re not doing enough testing. What’s the point of testing? It’s not going to make a difference anyhow. And that’s a very bad problem.
MODERATOR: Did you have a follow up?
Q: No. Great. That very helpful. I think that the trouble, especially in a state like Texas, was we’re hearing for so long with tests, we’re taking so long to come back that once that’s no longer the case or it’s improving, it’s hard to get past that original narrative.
BARRY BLOOM: I agree.
MODERATOR: OK, next question.
Q: Yes. Thank you, Dr. Bloom. I wonder if you’re familiar with antibody based therapeutics and might be willing to speculate about their potential, or any reservations you might have?
BARRY BLOOM: I’m pretty enthusiastic about monoclonal antibody therapies. As you will remember, one of the interventions in Ebola was the use of two monoclonals from Regeneron, which has been one of the companies pioneering monoclonal antibodies. They have some terrific advantages, they have high affinity antibodies that are not totally picky on amino acid sequences, so they don’t fail to react if there’s a very slight difference in the site to which they directed. The concept is, instead of waiting for someone to get a vaccine and wait 10 to 14 days to develop a primary antibody response, then 28 days later or a month later after that, to get a booster, this is already ready made antibody. It’s already been screened for high affinity. They’ve gone through thousands of B cells and monoclonal antibodies to get those that are high affinity. So they work the minute they go in, or within a matter of hours.
The second point is that there is always a worry with a monoclonal antibody. My lab actually made the first antigenic mutant of measles virus using a monoclonal many years ago. If you select against a single epitope, a single region of a protein, with a really powerful antibody selection, you basically select for mutants that have lost the site that are trying to get the virus to survive despite what you’re doing. So what Regeneron has done, and I don’t know whether Lilly has done, it’s trying to Regeneron has decided they would screen with two antibodies that see the receptor binding part of the viral spike protein, but they see different parts of that protein. They don’t overlap. So if a mutant was selected by one, the virus would be neutralized by the other, which I think is a brilliant strategy, anticipating a potential problem that hasn’t arisen in the real. And they’re obviously in testing for safety and efficacy in clinical trials now. Hopefully we’ll have results by the end of the summer. Lilly has also made monoclonal antibody. I believe it’s a single antibody at the moment, and another number of companies have made monoclonal screen monoclonal antibodies that neutralize this virus. So the advantages are, it’s already preformed. It’s preloaded and it can be used not only to perhaps treat people with early stage disease and possibly prevent it from getting out of control and leading to serious cases. It can be used to prevent infection in people who were contacts. And in fact, the trials that are being done are testing a variety of household and non household contacts to see if the antibodies protect against infection. If they did, it would have tremendously great value.
Two disadvantages. One is, it’s hard to produce a lot of antibodies on a on a scale that we’re talking about. This is mammalian cell culture and expensive. The second is, these are antibodies. They’re not yours. They’re somebody else’s. So they have a Half-Life and they dissipate over time because there’s no continuing source of that antibody unless you get another shot. That’s determined to a large extent by a portion of the molecule called the FC, which is not the binding site of the antibody, but has to do with how it’s handled by cells in the body. And there is evidence in other systems that you can put a region on a monoclonal antibody from humans that will extend its life within the body of humans by up to six months. So I would assume that what we’re seeing now are good. But if they work well and are safe, which there’s no reason to believe they wouldn’t, they can be made to extend longer. So instead of boosting every month with a new shot or every three months, might twice a year, be as good as a vaccine. And the third thing that they can do for us is, if monoclonal antibodies to the binding sight of the S protein is fully protective in people that we know that are exposed household contacts, then it tells everybody who’s making a real vaccine to immunize you that that becomes an assay to see whether their vaccine induced comparable protection against the same determinants. And that sets a standard that says if a monoclonal against this protein works, a vaccine that generates antibodies within you to the same determinants should also work. That could really speed up testing or vaccines without having to do massive clinical trials against disease. But just showing your vaccine is as good as a monoclonal having shown that the monoclonal absolutely. 100 percent protects against disease. So this is a really important innovation at a practical level, preventive level. It is unclear when in the course of people who are sick, antiviral antibodies are going to work, and at what point the immune system goes out of whack so you could get rid of all the virus, but still have to put people on ventilators because of the cytokine storm. So there’s an enormous amount to be learned about how to use these monoclonal antibodies if they do work, particularly in therapy, and that’s not yet clear.
Q: Excellent. Thank you. Really quick follow up. And I think you touched on this. Would any success with vaccines make this whole field of research moot, do you think?
BARRY BLOOM: Would what?
Q: If we’re successful with vaccines and that’s a big if. Would this field be rendered moot? Do you suppose?
BARRY BLOOM: No, I don’t think so. I think there will still be cases in which one has an exposure and perhaps not time enough in individuals in a nursing home, for example, and elderly people who don’t respond well to vaccines don’t give good immune response. As you remember, for flu, you have to have a higher dose if you’re in my age category. So this could be used instantaneously to provide protection in people who are unlikely to respond well to vaccines. People with immunodeficiency. People with cancer. People under other therapies. So if they’re good, I’m not sure I would bet that companies would make billions and billions of dollars, but no one’s ever made billions and billions of dollars on vaccines relative to therapeutics. So this is to save lives. And I think it will stay in the repertoire, and I hope it does.
Q: Thank you so much.
MODERATOR: Next question.
Q: Hi, can you hear me OK?
BARRY BLOOM: I can.
Q: OK. All right. Thank you, Nicole. Thank you, Dr. Bloom. I just wanted to also ask about turnaround times for testing, if I could. We learned today that recently the Massachusetts Department of Public Health, just in an effort to get residents there tests quicker, has asked providers who are conducting testing to work with the state to find that new lab partner if they can’t turn around their results within four days and to even discontinue their testing if they can’t do so. So my question is, you know, at this point in the pandemic, is four days quick enough for people to be getting their test results and for officials to be conducting contact tracing to try to prevent outbreaks?
BARRY BLOOM: My view is no. The sense is that the period of infectiousness appears to be greatest within two days of any clinical symptoms. So that is the time that most people don’t volunteer to be tested because they don’t think they’re sick. And then the period, once they think they’re sick, that they have to a large extent spreadable virus goes down from there as their immune response begins to kick in. So a test five days later, in my view, is essentially useless. It’s not that they’re not shedding after five days, but the amount of shedding is probably low enough that if people walk around with masks and distance, it’s unlikely to be a major source of transmission. So the question is how to hit people early on and how to get a result quick enough to find out how to find the chain of transmission, the contacts and phone calls and isolation, all of which does take time.
So I think four days is not acceptable from my point of view, from a public health point of view, it’s got to be 48 hours. And ideally, if that do it yourself for rapid tests are available at the first step, that could be done right away if they’re positive. You know, you’ve got a fair amount of antigen with the other tests, you have a fair amount of RNA if they’re negative. It doesn’t mean that you don’t have virus. It means you don’t have a lot of virus. Then you have to decide whether you would go for a PCR test and that would take an enormous load off the PCR test at the moment.
Q: Thank you.
MODERATOR: All right. Next question.
Q: We’ve been hearing rumors that some people may be asymptomatic or mildly symptomatic because of either previous infections or vaccinations. What do you think about the likelihood of that? Have some of us seen this virus before or something like it, and therefore, we’re protected? And why not everybody, if we’ve all had a common cold?
BARRY BLOOM: So that’s a really hard question because this really little definitive evidence. This is one of those areas I started with where there aren’t data to allow any kind of certainty. It arises because we all have exposure to common coronaviruses that cause respiratory infections. And what people early on in this epidemic did is obviously said if you had the common cold virus frequently, you must have antibodies to the common cold virus, which many, if not most people do. Do those antibodies protect against COVID-19, SARS-CoV-19. And the answer is to an overwhelming extent. They do not. They do not neutralize. They bind to the receptor binding site and appear not to be protected. What raised this issue, however, is that there is some evidence that at the T cell level, the role of which in COVID-19 is very unclear at the moment, there is some cross reaction in some people at the T cell level between the new virus and common cold viruses. Not everybody’s T cells show that. Nobody knows if those T cells are helpful or not. Nobody knows whether if you have T cells to a prior virus, whether they enhance or accelerate the production of antibodies by B cells that will speed up the production of a neutralizing antibody, or whether they are not likely to enhance production protection. But if things get out of control, it might be exactly those T cells that help antibodies that lead to the cytokines storm. We don’t know the answers to any of those ifs, but there is evidence of some degree of recognition in some people at the T cell level of cross reactive determinants between the COVID-19 virus and common cold viruses. And I’m sure there are lots of labs trying to track that down. It’s not an easy question to delineate.
Q: Thanks. And the evidence or some comments that link to the BCG vaccine might provide some protection?
BARRY BLOOM: BCG vaccine. My favorite vaccine. It’s a kind of interesting press story. The question that’s an issue is we talk about the specificity of immune responses. Landsteiner won the Nobel Prize showing that immune responses were not mysterious, they had chemical specificity and needed did a lot of chemistry to show how specific they were. We try to get antibodies specific to the spike broken. Well, we try to get T cells specific for tumor antigens. There has in the last 10, 15 years been this phenomenon of innate immunity, where there is a level of response prior to the ability of B cells to be amplified, T cells to clone, where the body has natural responses to infectious threats. The simplest case being production, for example, of interferon, common in virus infections. Viruses trigger a whole variety of cells, fibroblasts, macrophages, dendritic cells, nk cells, to produce interferons. And viruses have adapted as flu has, to not trigger the interferon that protects other cells against virus infection. So there are these innate responses.
So a number of groups got the bright idea, are there ways to enhance innate responses? And there is certainly evidence that BCG, which is a vaccine used against tuberculosis, protective in some parts of the world, totally non protective in other parts of the world, has the ability in people who’ve been vaccinated in particularly African countries against TB with BCG. If you follow them up, they have a tremendous drop in other respiratory infections, both bacterial and viral. And that’s called nonspecific or a reflection of some innate effect of BCG, not just against TB and specific antigens, but pumping up the immune system in general. An awful lot of the data on this comes from one laboratory in the Netherlands, which worries me. But they have led the fight. It has enabled The Wall Street Journal, The New York Times, two long reviews in Science and Nature without any real data to show that it would do the slightest thing to COVID because there are no data. What it did justify is attention to innate immunity and enabling clinical trials to be undertaken. There are trials in the Netherlands of BCG against COVID in health care workers and the same in Australia. And the expectation was, when they were begun, that by the end of the summer we would know whether BCG had a nonspecific effect in enhancing resistance by whatever mechanism against COVID, too. At the moment, these are great ideas. They work in mice and we really don’t have any data.
Q: Thank you.
MODERATOR: Next question.
Q: OK. Can you hear me now?
BARRY BLOOM: Yes I can.
Q: OK. I have a question about potential timeline for vaccine approval and wide availability. In some of your previous forums, you have discussed the idea that maybe one of these phase three trials produces acceptable results by the end of this year, and that it could be as late as the next year before it’s widely available. I guess this is sort of a granular question. But what happens in that interim? Do certain people start getting it according to the standards that are set by the federal government who are at higher risk of whatever they determine, and then they start expanding the population? Sort of the nitty gritty of getting to the point where it’s widely available in the U.S. and hopefully the world.
BARRY BLOOM: Really good and important question. I’ll tell you what I know. The good news is serious people have thought about this pretty early on. One of the things that is unique in this COVID vaccine business, a number of major companies have committed to producing at scale. Hundreds of millions of doses of vaccine without knowing whether the vaccine is safe or effective and approvable by the FDA. That’s never happened before. This is referred to in the newspapers as production at risk. If it is not safe and not effective, they’ve invested millions or maybe even a billion dollars building a factory, and their vaccine is not going to be approved. So that’s never happened before. And that is anticipating that some, and I would guess most of those that are being in phase three studies now, that have shown immunologic production of antibodies that neutralize the virus in a test tube and have some likelihood of generating protective immune responses. I think that the government’s bet is that many of them will have protective efficacy and the role of the Phase three trials with thirty thousand people is to find out. Are they better than 50 percent efficacious? Do they prevent 50 percent of people from getting the disease? And are they safe and 30,000 people, when you’re really concerned about uncommon adverse effects that are not seen in a hundred or a thousand people, but could be very serious. And so that’s why I think there have been big investments both in the companies and in the government that some of these platforms. Past experience with Ebola and influenza and MERS suggests that at least in small studies, they produced immune responses pretty well. They didn’t have big safety issues. They, at least some of them and maybe most of them, will work. And the question is, how well would they work? So that’s the first part. I’m pretty optimistic that most of them that are in the frontlines are likely to have a good efficacy. Ideally, from my point of view, I’d be thrilled if it was in the 70 to 75 percent range. Expecting the effect of measles, which is 94 percent protective, is asking an awful lot in seven months to create brand new vaccines from Earth, air, fire and water.
The second part of your question is going to be a vexed issue given the massive distrust of vaccines in this country, which is relatively but not unique totally to the US, is linked with the distrust of anything the government does. Who’s going to get the vaccine first? And forgetting politics, which I won’t get in, there are really two issues, two completely different strategies that somebody has to think about. And I’ll tell you who’s been charged to think about. The obvious one that most people would do would be the ethical argument that people most likely to die, whose lives are at stake, should have highest, first access, high priority. That would probably include health care workers that are dealing in ICUs with COVID patients, nursing homes, prisons, possibly schools and college students, schools with children, if that would seem to be a problem, and essential workers that have to be out interacting with the public. So that’s one set of categories of who would be priority for highest risk for death and serious illness with this disease. The public health perspective would be, who are the transmitters that the name of the game in infectious diseases is in a sense, keeping people alive is secondary to interrupting the transmission of a lethal pandemic disease and making it go away. So you would focus the public health emphasis on the transmitters, and that’s where students, college students, essential workers might figure in to a different priority.
What’s interesting, and I will recur to politics. Let me just say that the priorities for all new vaccines, the mechanism that’s been used for the last 30, 40, 50 years, has been a committee convened under the CDC, with people outside the CDC, called the ACIP, the Advisory Committee for Immunization Practice. They recommended doses, they alert pediatricians for adverse effects, and they have traditionally decided how vaccines would be allocated to get them out there till there is enough in this circumstance. The director of NIH and the director of CDC asked the National Academy of Medicine, which is now involve the entire National Academy of Science, Engineering and Medicine, to convene a committee to hold public hearings. There have been two thus far. They will continue into the fall. They’ve charged this independent committee to make recommendations to whom is less than clear, clearly to the public, the National Academy reports to the public. But they are charged since 1865 by Abraham Lincoln to advise the government of the United States, on matters to do with science. So I am hopeful that they will make a set of recommendations based on testimony from interest groups, from patient groups, from health workers to come up with a justification for a set of priorities. That, of course, in America, not everybody will subscribe to, but will at least indicate it was as fair process as possible, in consideration.
I put that in the context where the concern is that when the CDC put out a report on opening schools, there was intervention from the White House to prevent their recommendations for becoming public. And hence, I believe that this was done to assure the public that this would be an independent committee based in the National Academy of Sciences to do the fairest openness job that is as resistant as it exists in America, free from political intervention. So that’s the second step and we would expect to have hopefully by late October, mid-November, sometime like that, when there might be vaccines just becoming available. Those recommendations would be put forward. And the CDC, which really is engaged with how to get vaccines from the producers to every district in the country, would have to pick the ball up from there. The hope is that people would find those reasonable and accept that they have been done in the fairest way.
The next step, then, is when companies have promised they will have 300 million doses, which would cover all of America with one vaccine by the end of 2021. There is good reason to believe if all of these top six vaccines, for example, were safe and effective, we could get a lot of vaccines out, even though very few companies could do the whole country if they were all approved by January 1st. I would guess in six months we could get those to almost every part of the country. The difficulty here is most vaccines that we know how to distribute and we do know how to do that. CDC has done that well through the Association of Immunization Managers in every state and the state and territorial health workers, this is an infrastructure people don’t know about. They get their vaccines in the schools. They keep a record of every school that gets vaccinated so that they know if there’s an outbreak, they could predict what schools haven’t had enough coverage in their vaccines. They’re not so used to delivering vaccines for adults. They sure don’t have a history of working in nursing homes and prisons. So there’s going to be a lot to be learned to answer. The third part of your question of how do we distribute these once the priorities are set? The vaccines start to become available. How do we get them to the right places? How do we keep records on the people who had them? And how do we follow up for longer term adverse effects that may not show up in the three months, in the early testing, even though the statistics say they’re protected? How do we get so-called post licensure surveillance? To be sure, two years from now, we know there were very few adverse effects and they really did work. Long answer to a very important and challenging question.
MODERATOR: Do you have a follow up question.
Q: Yes, real quick. Two quick things. And I just want to make sure I heard you right. It’s not clear who the National Academy of Sciences will make their recommendations to. And secondly, from the process you described, it seems like if they’re all OK, you could have available vaccines for most of the country by mid year. But if not, if there’s less, probably later in the year?
BARRY BLOOM: I think that that’s right. I think we can pretty well be assured, assuming that they are safe in these phase three trials and the companies are willing to produce at risk before they get these answers. The way that it’s worked is that the government, the NIH, BARDA, have offered the following. They are paying many of these companies to produce 100 million doses with an option that if they work well and the government needs five hundred million for, let’s say, two shots, you have to double the amount of vaccine the government has taken options on. In the other case with Pfizer, what they have done, Pfizer asked no money, as far as I know, to develop the vaccine from the government. What they’ve asked is an advanced market commitment. If we have made 100 million doses and it is safe and effective, we need you to guarantee you’ll buy 100 million doses. And the government has committed to doing that. So those are two mechanisms we’ve never had before, designed to really get the scale of acceptable vaccines up to speed in an unprecedented way. And so I’m pretty hopeful that many of the vaccines will meet the safety and efficacy criteria, that whatever the recommendations of the academies will be reasonable.
Where I’m most concerned is that people won’t take them. That the misinformation, whether it’s introduced from overseas or from conspiracy groups, will dissuade people, have them believe that the safety criteria, because it’s passed, has been compromised. And the safety criteria and the efficacy criteria are statistical. They depend on how many people are being tested, not the time. Time is not a variable in that calculation, other than any long term adverse effects. So everyone has said, NIH, CDC, and the director of the FDA multiple times, including today in The New York Times, there will be no shortcuts taken on safety and efficacy. And what’s at stake here is not just the COVID vaccines. If there was anything bad that happened with a vaccine that was approved like hydroxychloroquine or the useless antibody tests that were allowed to go forward under emergency use, the credibility of all vaccines, childhood vaccines would crash. The outcome would be catastrophic, in my view, for the health of people in this country. I hope the director of FDA and the head of the Department of Health and Human Services will not allow anyone at any level, government or outside to compromise that decision.
Q: So is it Health and Human Services that will make the final decision? You’re not sure?
BARRY BLOOM: Well, it’s FDA that makes the decision. And FDA is part of of HHS. FDA has traditionally had multiple levels of the committee, its top two guys sitting in the director’s office. They generally go through a month or more on a new vaccine of data. And that leads to the possibility if the data say it’s safe and effective, it may still take a lot of time for expert committees and levels within the FDA to get all the statistical stuff to be sure that they’re not missing anything, which they do for every vaccine. So they may have to issue an emergency use for a month or so, till the final approvals are done. I hope that doesn’t have to happen because there’s enough suspicion about emergency use authorization. One would like to have genuine, careful, full scale review, full scale approvals. That would be my view.
Q: Thank you.
MODERATOR: Next question.
Q: I just had a real quick follow up to that question on timeline again. Recently, the president had said he was optimistic that there would be a vaccine ready by Election Day. In your estimation, is there any chance of that happening?
BARRY BLOOM: I wouldn’t bet against a press release from one of the companies assuring us that their vaccine has met all the standards by Election Day. I hope that doesn’t happen. It’s very hard for me to imagine that there would be sufficient data and time for data analysis at the FDA to get it all done by November 3rd. I think it’s not impossible for the trial to reach the endpoint. The endpoint is the statistical number of people in the trial who get sick. And that’s when you say you can stop the trial, we have statistical power. Now, how many of those were in the placebo? How many of those got the vaccine? And was the vaccine 50 percent or better protected? It’s not impossible that that endpoint could be reached for a couple of vaccines by November. It’s not conceivable to me that a detailed analysis of all of the data and review at multiple levels of FDA could be done by that. But we shall see.
Q: Thanks.
MODERATOR: I think that’s our last call. Do you have any other thoughts, Dr. Bloom, before we go?
BARRY BLOOM: No, thank you all for the very good questions. I would just throw in an answer that I didn’t make before, that I haven’t heard raised by any of these press calls that I think is a serious issue, and I’m trying to find out more so I don’t have answers. Once the vaccines are mad, and they have to get out to, whether it’s doctors offices or health departments for distribution, there has to be a cold chain. And some of the vaccines have to be kept at minus 20 degrees centigrade and the RNA vaccines, or at least some of them, may have to be kept at minus 80 degrees, which is freezer or dry ice temperature. I’m not sure we have a distribution system in the past that has been asked to accommodate that level of security of the vaccine being preserved at those temperatures. And that’s going to be an engineering trick that I know people have to be worrying about. But I don’t know who’s worrying about it and how secure they are in being able to get the companies to be sure their vaccine is in 100 percent good form by the time it hits the nursing home in Phoenix, Arizona. That’s something that I think if you’re asking people, more knowledgeable than I, is an important question to do.
This concludes the August 11th press conference.