Improving radiation therapy for cancer
October 17, 2024 – Around a decade ago, Sean Murphy was living in France, pursuing a professional soccer career—“somewhat unsuccessfully,” as he put it. One day, he suddenly started experiencing symptoms including nausea, headaches, and vomiting. When he went to the hospital, a CT scan showed a lump in his brain that required immediate surgery. He was eventually diagnosed with a brain tumor, and underwent treatment.
“Treatment went well—the tumor regressed. Essentially, my soccer career was over, and I was looking ahead toward my first year at Harvard,” said Murphy, who spoke at the 27th annual John B. Little Symposium, held Oct. 11 at Harvard T.H. Chan School of Public Health.
At the symposium, researchers discussed a wide range of advances in radiation therapy for cancer. Murphy offered a patient’s perspective.
Partway through his undergraduate studies, Murphy went to the doctor for a routine checkup—and found a recurrence of his cancer, which soon metastasized. Because the cancer had developed resistance to previous therapies, treatment needed to be harsher, with the potential for serious side effects.
“There was a difficulty for me in deciding exactly what kind of treatment I wanted to do, because I had to strike a balance between quality of life and efficacy,” he said. “So I invited some of my smartest friends at Harvard to a medical hackathon.”
Together, Murphy and his friends analyzed cancer studies to come up with the best treatment approach. “The most reassuring thing happened, which is that [my doctor] brought out the same [research] papers I had,” he said. They decided on a treatment plan that included different types of radiation, chemotherapy, and a stem cell transplant. Now in remission, Murphy is pursuing a PhD at the Massachusetts Institute of Technology.
“What you guys are doing, the research you’re doing, is impacting people every day,” he told the audience.
The symposium was hosted by the John B. Little Center for Radiation Sciences, named for the late John B. Little, the former James Stevens Simmons Professor of Radiobiology, Emeritus. Organizers of the event included JBL Center co-directors Zachary Nagel, associate professor of genomics and cancer biology, and Kristopher Sarosiek, associate professor of radiation biology and cell death; along with Henning Willers, associate professor of radiation oncology at Harvard Medical School. The JBL Center has been a pioneer in the field of radiation research since its establishment at the School as a result of the philanthropy of Gerald Chan, SM ’75, SD ’79.
“By including perspectives drawn from mechanistic, computational, and translational studies, the symposium embodies a theme that resonates with one of the greatest strengths of our School—bringing together an array of disciplines and modes of research to address public health problems, which are always complex,” said Andrea Baccarelli, dean of the faculty, in his opening remarks.
Artificial intelligence for cancer care
AI has the potential to improve cancer care across a broad range of areas, such as diagnosing tumors, determining the most effective treatments, and predicting the risk of recurrence, according to Hugo Aerts, an assistant professor of radiation oncology at Harvard Medical School.
One AI method that Aerts has developed is FaceAge, an algorithm that analyzes a photo of a person’s face to predict their biological age, a factor that influences cancer outcomes. Due to lifestyle factors such as diet, stress, and smoking, people age at different rates, so chronological age measured in years might not correspond to the body’s age on a biological level. Using the FaceAge algorithm, Aerts and his colleagues found that the biological age of cancer patients was generally higher than their chronological age, and that biological age could better predict survival time. The researchers also found that in patients receiving palliative radiation therapy, FaceAge improved predictions of survival time when combined with clinical information that is currently used for treatment decisions, such as cancer type, previous treatments received, and number of hospitalizations.
“There is something being captured in a picture that’s not being captured by other parameters that we have,” Aerts said, adding that the algorithm could help patients and clinicians to evaluate the potential risks and benefits of treatment.
Aerts also highlighted challenges in the field of AI, such as making sure that models being developed have a clinical impact. “There’s a lot of great stuff being published, but not a lot makes it into the clinic. We call this the translational gap,” he said.
Additionally, Aerts—who is director of the Artificial Intelligence in Medicine Program, which brings together researchers across Harvard-affiliated hospitals and schools to share software and promote collaboration—noted that there is a great need for more sharing of AI code and data among researchers. “There’s a reproducibility crisis in AI,” he said. “There’s a huge problem that we face in the field—a big need for transparency.”
Positives and negatives of radiation therapy
Other symposium speakers included Sandra Demaria, a professor of radiation oncology and pathology and laboratory medicine at Weill Cornell Medicine in New York City. She studies the mechanisms of how radiation therapy improves the immune system’s response to cancer.
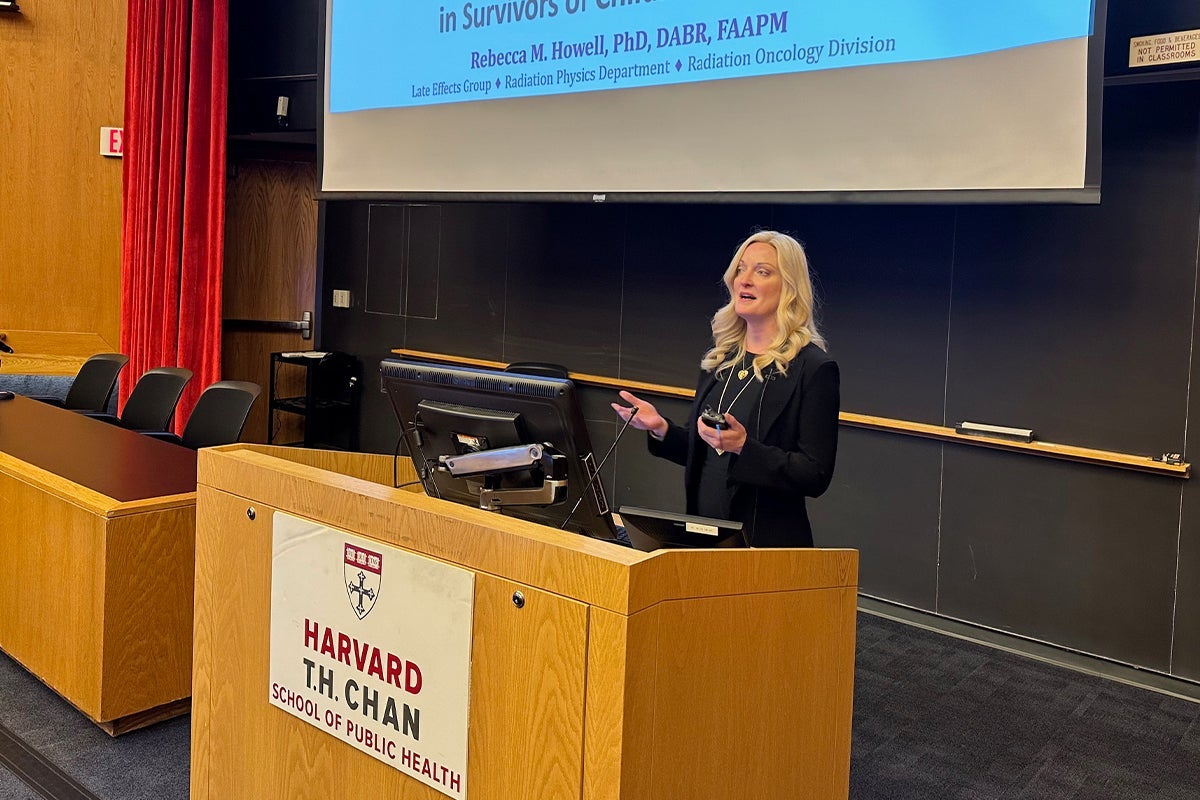
Rebecca Howell, a professor in the Department of Radiation Physics at the University of Texas MD Anderson Cancer Center, shared her research about the long-term negative effects of radiation therapy in survivors of childhood cancers. In particular, cardiovascular disease is the second highest cause of death in survivors, she said. Howell has developed computational models to analyze how radiation to different parts of the body can result in an off-target dose to the heart, leading to a risk of cardiovascular disease years or decades later.
– Jay Lau
Photo: Zachary Nagel