Coronavirus (COVID-19): Press Conference with Sarah Fortune, 03/26/20
Transcript
You’re listening to a press conference from the Harvard T.H. Chan School of Public Health with Sarah Fortune, the John LaPorte Given Professor and Chair of the Department of Immunology and Infectious Diseases. This call was recorded at 11:30 am Eastern Time on Thursday, March 26.
Previous press conferences are linked at the bottom of this transcript.
SARAH FORTUNE: Good morning. I’m Sarah Fortune. I am the chair of the Department of Immunology and Infectious Diseases at the School of Public Health. And I am happy to be here this morning to answer your questions.
I thought I would begin with a sort-of four-minute introduction, both of myself, and then to give you an idea of what I’ve been thinking about recently. And I promise this is going to end up on COVID and COVID – where we are in terms of COVID control locally.
The place I’d like to start is actually my area of expertise. I study tuberculosis. And I’ve spent my career studying the intersection of the biology, the intervention for tuberculosis, and global health systems. And as some of you might know, TB is actually the leading cause of infectious deaths in the world. There are a million people who die of TB every year. And I think we all have a better sense of what that looks like in the setting of this COVID epidemic.
And Tuesday was World TB Day. Normally, we spend that day celebrating our accomplishments and looking forward to what we need to do. But this World TB Day was marked by virtual meetings, trying to understand the impact of COVID on TB control. And in one of those virtual meetings I had the opportunity to hear from a journalist actually, Vidya Krishnan in India, who has spent her career documenting the fragility of the Indian health system and its inability to take care of TB patients in India.
And as you know, I think, India is the second most populous country in the world. It has the largest burden of TB cases in the world, so about a 1/3 of the 10 million cases every year. And its burden of TB is a very good metric for the fragility of its health system. And so Vidya both describes the terrible plight of TB cases in India, but also to the state of COVID control in India.
So, they report only about 700 cases, but they basically have tested no one. They have no PPE. They have no medical infrastructure. And they have an increasingly fraying social fabric, in her description, where doctors are being evicted from their homes because there’s big concern that they are vectors of contagion.
And so, listening to her really quite dire reports from India, I was reminded that this tsunami that is facing us all is facing – is coming to countries with really very fragile health systems that have very little capacity for dealing with it. And that, really, to witness the limits of what we can achieve even locally in terms of COVID control are set by the globally – set by the weakest health care systems globally.
And so, when we think about what we’re trying to do with something like social distancing, I think it’s appealing to think about the Chinese model, where China was exceptionally successful in using quarantine and social distancing to drive the genie back into the bottle. But I think we have to be honest that the genie is out of the bottle. And globally, we’re using these tools, as everybody understands, to flatten the curve, but really, probably not bend the curve back to zero.
And so, as I was entertaining these dark thoughts on Tuesday, there was a paper by Yonatan Grad, who’s a junior faculty in the Department of Immunology and Infectious Disease. It’s Kissler, et al. It’s on the pre-print service, which I highly recommend you look for. But it provides a roadmap for thinking about how we can flatten the curve. But we are going to have to let the epidemic play out in such a way that we do achieve enough herd immunity to protect us against catastrophic recurrences of the epidemic.
And so, he proposed a model in which you basically tune social distancing and intervention, to tune to the capacity of the health care system in order to try to save as many lives as possible, while preventing the subsequent waves of epidemic transmission. And I found this – and this really just depends on four things – medical capacity, which is PPE, beds and ventilator, and tests.
And so, I want to end the introduction with the really optimistic numbers from the State of Massachusetts in terms of testing, since you’ve all heard about the limitations of testing capacity. And in the State of Massachusetts, yesterday, they are between – on the 25th of March, we performed 6,000 tests. So, our testing capacity has gone up from about 250 tests a day to 2,000 tests a day, to 4,000 tests a day, to now, we’re performing 6,000 tests a day. And I believe by the end of the week, there’s an estimate that we will be at 8,000 to 10,000 tests a day. So, I think there is a glimmer of hope in terms of the testing capacity coming online to be able to let the epidemic play in a controlled fashion and hopefully, save as many lives as possible.
OK, so I’m happy to take questions based on that.
OPERATOR: We do have our first question.
Q: Hi, Prof. Fortune. I just want to make sure I understand you right. And you know, this is a potentially important message for the public to get, that the point of everything we’re doing now is really not to avoid getting infected entirely because that wouldn’t do anything to raise herd immunity eventually and put an end to this, but to manage it in a way that as many lives are saved as possible. Is that right?
SARAH FORTUNE: I believe that that is the most realistic path forward. I believe that there has been some vacillation in domestic policy settings, trying to understand whether we could achieve what China achieved, which was not just flattening the curve but really driving it back to zero, so putting those – as I like to think of it, putting the genie back in the bottle, or whether that is functionally – now that is a global epidemic, functionally impossible, and what we are trying to do is control it in such a way that we can save as many lives as possible. And I believe it is the latter which is the most realistic path forward now.
Q: And is it likely, when we look at places like Africa and India, where, at least from a testing standpoint – and we don’t know what the real case is – it looks like the epidemic is arriving and starting to grow, do you have a sense that, even here in the US, we will see separate waves that, regardless of what happens over the next four months with social distancing and everything else, that a year from now, or 18 months from now, absent a vaccine, of course, that we’ll be dealing with this again? Or is it impossible to tell?
SARAH FORTUNE: So, absent the vaccine, I think it is clear that we are going to be dealing with separate waves. Now, what the timescale of those waves are is not entirely clear.
But when people talk about the transmission of the virus, obviously, transmission is both dependent on the number of cases in your community but also the density of the community. And so, the way a wave rolls through your community depends on local factors. And we can intuit that now because you understand what’s happening in New York versus Wyoming. And so, the progression of transmission is going to look different in different communities based on density.
And I think that – actually, this is a separate thought. There could be a much more coordinated federal distribution of resources if we understood that resources need to be distributed based on the different density-dependent temporal factors that are going to make the burdens hit in different communities at different times.
Q: Thank you.
OPERATOR: Next question.
Q: Hi. Ski resorts, national parks, the Disney resorts, those are all doors for people around the country and around the world. It means that there’s a lot of social mixing that happens in them. Yet a lot of these places did not close down until late into this crisis. I’m in Colorado. I’m thinking in particular of our ski resorts. They didn’t close until March 15, which was a while after Colorado began tracking cases, confirmed cases, after ski towns themselves had started to have outbreaks. Was that a mistake to wait so long to close these places down?
SARAH FORTUNE: You know, I don’t want to really second guess anybody in this because I’m not sure that second guessing helps moving forward. And I think I actually – I think at a point in time when we thought we could eliminate the virus, eliminate transmission, and rid it from our communities, like China functionally did, then the earliest – shutting down at the earliest moment possible would have been the ideal.
But given that the virus has taken hold in our community, I think we’re going to have to accept that we’re not going to be able to rid our communities of virus, and therefore, the discussion should turn to how can we have moderate and sustainable social distancing to slow it, but not expect that we’re going to eliminate it, such that we can save lives, right, but that’s a ski resorts or the communities will be able to function at some level. In an ideal world, it would be sort of moderate and tunable social distancing.
Q: All right, thank you.
SARAH FORTUNE: Yeah.
OPERATOR: Next question.
Q: Hi. I was wondering if you could talk a little bit about serological testing and how this could help us better understand the epidemic. And are there any other countries that have that capacity?
And then I was also wondering about mitigation strategies. Some advisors, particularly here in France, the scientific advisors have said it would last at least six weeks. Are there good estimates – do most epidemiologists believe that’s going to be a matter of months and not weeks? Thank you.
SARAH FORTUNE: So, let me speak to your first question about serologic testing because that is extremely important. So, as you know, the nose swab testing is looking for wide virus – or virus in your mucosa right now. And it tells you if you’re acutely carrying coronavirus, but it doesn’t tell you if you’ve had it or not.
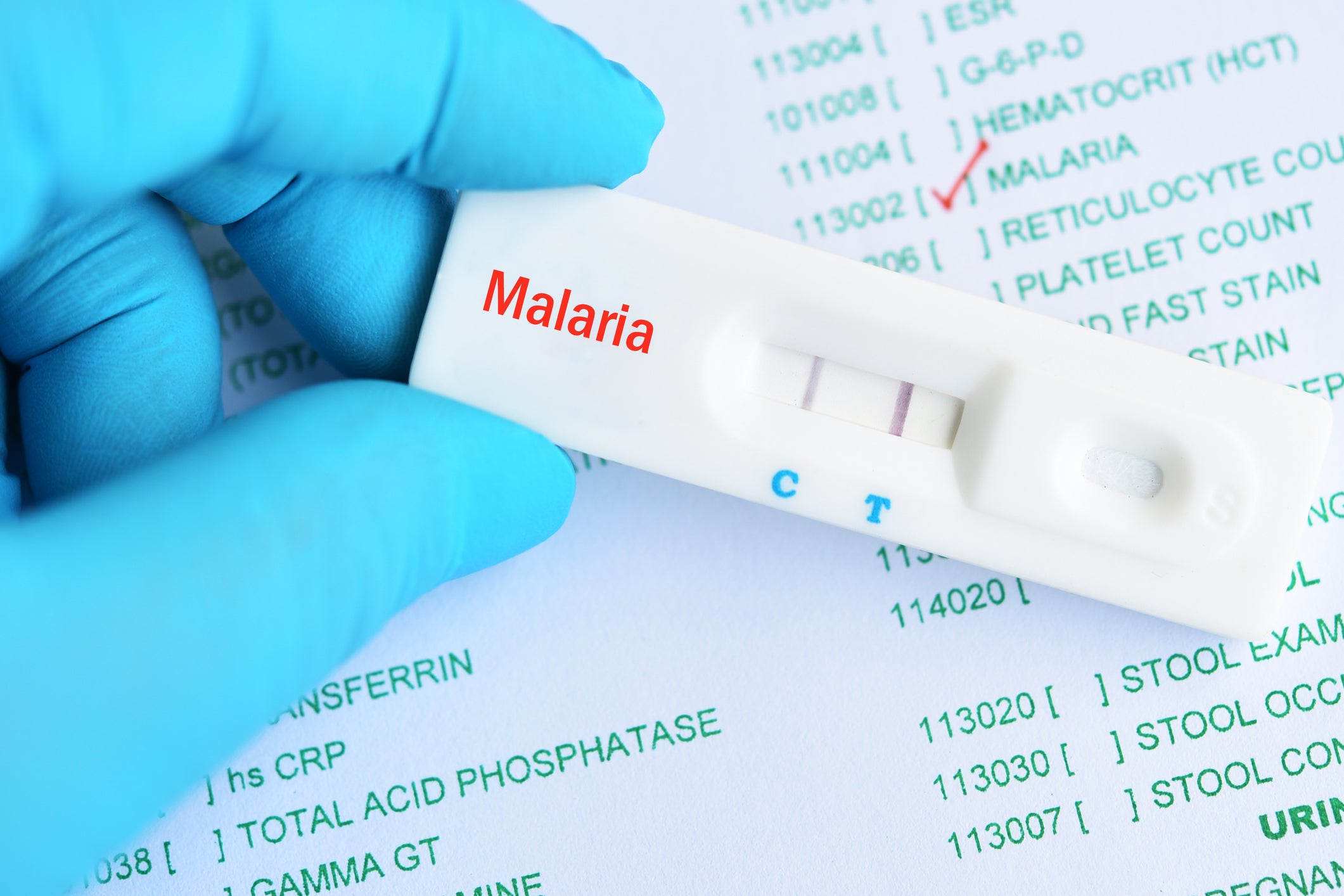
And serologic testing is a way to tell you whether you’ve had it, and in theory, have immunity to it. And it is – the important part about serologic testing is it’s much, much, much, much, much easier to deploy. And you can think about it as a sort of pregnancy-test-like deployment of it.
Serologic testing is being deployed in China. And there are other serologic tests. I’m sure that you have heard that the UK promises to roll out serologic testing on a large scale. And I don’t know the quality of those tests yet.
But I think it’s going to be an important way to try to understand where we are in the epidemic as it rolls forward because it helps us understand in a much more feasible fashion how we’re doing and whether we’re allowing enough progression, that we are getting enough herd immunity that we’re moving towards a protected population. So that’s the first thing. So serologic testing is critical. And at least in the United States, it is disappointing that it also appears to be lagging behind testing that has been available in China.
And the second point is, is it weeks not – or is it months, not weeks? And I think it’s obviously going to depend on local factors and where you are in the epidemic. I suspect that France is not over the hump in terms of the epidemic. And therefore – but something like a serologic could elucidate that. And if you knew where you were in the epidemic, you’d have a much better sense of whether it’s going to be weeks or months. In the United States, it’s clearly where we’re clearly not over the hump. It’s clearly going to be months, not weeks.
Q: Great. Thank you.
SARAH FORTUNE: Yeah.
OPERATOR: Next question.
Q: Well, hi. A couple of questions.
One is, could you give the name of the first author of that paper you mentioned, who wrote that for flattening the curve?
Second, what do we know about common cold coronavirus infection? Do they return every year like the flu and the swallows in Capistrano?
And also, when you’re saying that we need herd immunity, how do you encourage that while encourage everyone to be socially isolated? It’s just going to be a side effect of people – not everybody doing what they’re told? Thanks.
SARAH FORTUNE: Yeah. So let me answer that first and third question, and then the coronavirus question, OK?
So the author is Kissler. K-I-S-S-L-E-R, is the first author. And the last author is Grad, G-R-A-D.
In this paper, essentially what they propose is moderate social distancing, so not extreme social distancing. But once you are medically – all our infrastructure and our critical care resources are all in place, moderate social distancing, expecting that people are going to get infected. Some people are going to get sick, and some people are going to die. We need to save as many people as we can and limit transmission such as that as few people as possible get sick in order – but people have to get infected in order to get herd immunity.
And I guess that’s the roadmap they propose, so a roadmap where you do allow a little – when you’re ready, when your health system is ready, you do allow moderation of social distancing, expecting that you’re going to release transmission in order to build herd immunity such that you don’t, at a later date, have this cataclysmic pandemic again – you know, epidemic transmission again.
Oh, and then the seasonal coronaviruses, there are lots of these seasonal coronaviruses. And I don’t know enough about the transmission of individual seasonal coronaviruses to be able to speak to that very authoritatively.
Q: Any suggestions of coronavirus experts?
SARAH FORTUNE: Ralph Baric, B-A-R-I-C, at the University of North Carolina.
Q: Great.
SARAH FORTUNE: Yeah.
Q: OK, thank you.
SARAH FORTUNE: Yeah.
OPERATOR: We have our next question.
Q: Hello, yes. This is a journalist from China. And I long to ask the question about the symptomatic infection. It is said that the data on invisible infections is an important indicator of future decision-making and whether the COVID-19 will make a comeback, and how to respond if it did that. How do you think about it?
SARAH FORTUNE: You mean in China in particular?
Q: No, no, around the world.
SARAH FORTUNE: So OK, so to parse that into a couple pieces, clearly, one of the challenges about COVID and COVID transition is the relatively high proportion of people who are asymptomatically– and asymptomatic when infected and capable of transmission. And as I am sure you know, estimates suggest that about 40% of transmission is asymptomatic.
And it is very hard – a nimble public health system will be able to try to track, based on the appearance of symptoms back to asymptomatic carriers. But that is very challenging. And I guess that is yet another reason why I think it is probably in the absence of something like the incredibly heroic effort that was undertaken in China to track down asymptomatic carriers, which I do not think less robust health care systems are going to be able to do, I do think transmission is going to continue and that the epidemic is going to play out through the world.
And just mathematically, this is in a quantitative estimate. So, in the Kissler paper, they estimated that bringing transmission down to about 40% of unrestrained transmission would really significantly improve our ability to, at least domestically, take care of people, that basically capturing all the symptomatic transmission. And so, we would have to do a really good job of capturing all the symptomatic transmission and then accept that there is asymptomatic transmission.
Q: OK. So, what can be done about it? What will come next?
SARAH FORTUNE: What will come next?
Q: Yeah.
SARAH FORTUNE: You’re asking – I – yeah – you’re asking me to prognosticate. I don’t know what’s going to come next because it’s going to depend on the actions of the health care systems around the world. I do fear, however, that where health care systems are very fragile that what’s going to come next is actually the pandemic playing out in a really catastrophic way.
Q: Oh. Yeah. Thank you very much. Yeah.
OPERATOR: Next question.
Q: Hi, Professor Fortune, I would like to ask you whether the promise of chloroquine is real or not? Or if there is any other promise for any antiviral medicine that we can farm in a short time, before the vaccination.
SARAH FORTUNE: Those are excellent questions. And the honest answer is I don’t know. The data on chloroquine is really very preliminary, very preliminary data, where there is effect in experimental systems, effectiveness in experimental systems. And I do not know of any data suggesting that there is marked – showing an effect in clinical settings.
That said, I think that chloroquine, if it were effective – and I don’t know that it would be – I think what one could expect is a modest antiviral activity, but not – a modest antiviral activity might allow prophylaxis, like exposure prophylaxis and the buffering of transmission chains, which might have an impact on transmission and might mitigate clinical severity, although it’s probably unlikely to markedly improve the outcomes in people who do become very sick.
So I think that there are some therapies directed at the immune response, the destructive immune response, which are likely to have clinical efficacy in terms of the saving people’s lives if they’re very sick. But only a very few people are going to get access to those. And the same is honestly true for something like remdesivir, which is the Gilead antiviral, which is intravenous.
Q: Right.
SARAH FORTUNE: For the world, a vaccine would be the best.
Oh, and I do want to emphasize, chloroquine is very toxic. So, people should not just go out and randomly take chloroquine.
Q: Yes. Thank you. Think you so much.
SARAH FORTUNE: Yeah.
OPERATOR: OK, next question.
Q: I’m wondering if – to go to your point about how these waves are going to be moving through various states and local municipalities, and managing those death tolls related to surges past hospital capacity are happening in the very local context, what roles do these kind of various national and state level epidemiological models that we’re seeing being published in the last few days and few weeks – what roles do those models have to play in shaping local policies regarding physical distancing and managing the surge?
SARAH FORTUNE: I think those models are very important. I think local models are very important because I think that, actually, in an ideal world – and I’m not saying we live in an ideal world in terms of the US public health system. But in an ideal world, managing – interventions like social distancing would be driven by local data and driven by local hospital capacity. And there would be a sort of ability to respond very locally to the epidemic, recognizing that the epidemic in New York is not the same as the epidemic in rural Ohio right now, and that maybe the social distancing strictures could be tuned to your domestic condition.
And again, New York in August might actually be at a much different place than Denver in August, right, where New York might have gone through a wave much earlier, and Denver might be in a different position. And so, the ability to have local models – but it would be ideal if those could feed into a coordinated federal response. And of course, that is very distressingly absent at this point.
Q: Thank you.
SARAH FORTUNE: Yeah.
OPERATOR: We have our next question.
Q: Hello, Professor. Experimental results said the governments, that is, the US, for example, does it work? And can you tell us more about it?
SARAH FORTUNE: Does the government’s strategy – OK, I think I might be skating off into an area where I don’t have expertise that I should really be commenting, except to say that I think that the US government needs to move to a coordinated federal strategy. Right now, we’re seeing state-by-state strategies. And it would be ideal if we moved to a coordinated federal strategy on managing how we’re going to manage transmission, and if there were a unified message. But I think I should just leave that at that.
Q: OK. Thank you. Thank you so much.
OPERATOR: We do have a question.
Q: I was just wondering, when we say that it’s going to be 12 to 18 months for a vaccine, has that ever happened before? That would be incredibly fast, no?
SARAH FORTUNE: It would be incredibly fast. And I think that people should be cautious about what their expectations are in terms of a vaccine.
So, it’s one thing to develop a vaccine that works or it works in a small group of people. Then it has to work in a larger group of people. And then it has to be made, manufactured at a scale where it can be distributed to millions of people.
And those are – the idea that that can be accomplished in 12 to 18 months, I know people are working very hard to do that. But it should be recognized that those are very ambitious goals. And that has not been achieved, except we do make a whole lot of seasonal influenza vaccine every year, so it’s not impossible.
Q: Thank you, ma’am.
SARAH FORTUNE: OK, one more question, then I’ll go.
OPERATOR: One more question.
Q: Yeah, hello. I want to ask, can you tell us more about the antibody study? What does it contribute to the study of a vaccine?
SARAH FORTUNE: They are very – antibody studies are very important in understanding of the potential for vaccine-mediated immunity because most of our effective vaccines, it needs to correlate with the titers in neutralizing antibodies. And so there have been passive transfers of HeLa that suggests that the antibodies are protective. And I think that those studies, albeit preliminary, are optimistic in terms of informing our understanding of how hard or easy it will be to develop a vaccine.
Q: Yeah. OK, thank you.
This concludes the March 26 press conference.
Press conference with Caroline Buckee, associate professor of epidemiology and associate director of the Center for Communicable Disease Dynamics (March 25, 2020)
Press conference with Marc Lipsitch, professor of epidemiology and director of the Center for Communicable Disease Dynamics (March 23, 2020)
Press conference with Marc Lipsitch, professor of epidemiology and director of the Center for Communicable Disease Dynamics (March 20, 2020)