May 11, 2015 — More than a million HIV infections could be prevented over the next 15 years by increasing circumcision of uninfected men in the five countries in Sub-Saharan Africa with the worldwide highest HIV prevalence, according to researchers at the Harvard T.H. Chan School of Public Health. In addition, the survival benefits of increasing male circumcision coverage compare very favorably to the costs of the intervention. And while expanding anti-retroviral treatment (ART) is another highly cost-beneficial HIV intervention to improve survival, researchers found that circumcision has an even more attractive cost-to-benefit ratio.
The findings come from a new paper written for the 2015 Copenhagen Consensus, by researchers Till Bärnighausen, David Bloom, Pascal Geldsetzer, and Salal Humair. They argued that national governments and the international community should aim to increase male medical circumcision (MMC) rates to 90% of HIV-uninfected men in Botswana, Lesotho, South Africa, Swaziland and Zimbabwe. That target was one of 19 global health priorities selected by a panel of Nobel laureates among more than 100 proposals for the Post-2015 Development Agenda by the Copenhagen Consensus, which brought together the world’s top economists to identify the “best buys” for development. The 19 selected global health priorities are the Copenhagen Consensus proposal for the United Nations’ next development agenda, which will be set by the UN General Assembly in September.
Till Bärnighausen, associate professor in the Department of Global Health and Population, says that circumcision offers large value for the money.
“It’s cheap, and it can be done safely, including by nurses and clinical officers,” said Bärnighausen. Additionally, there is widespread acceptance that circumcision is effective in preventing HIV—clinical trials have shown that circumcision leads to a greater than 50% reduction in HIV acquisition risk.
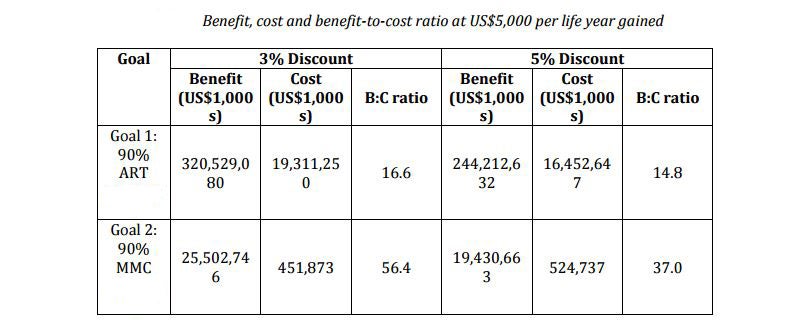
The researchers used a mathematical model to compare the benefits and costs of circumcision to other HIV interventions, including the expansion of ART for those already infected with HIV. They found that while life years gained were more than 10 times higher for ART than circumcision, the cost of scaling up circumcision was much lower: about $500 million to increase circumcision coverage to 90% of uninfected men compared to more than $15 billion to expand ART to 90% of individuals currently needing the treatment. However, both circumcision and ART are highly cost-beneficial and they benefit different populations—which is why the researchers recommended both interventions in their contribution to the Copenhagen Consensus.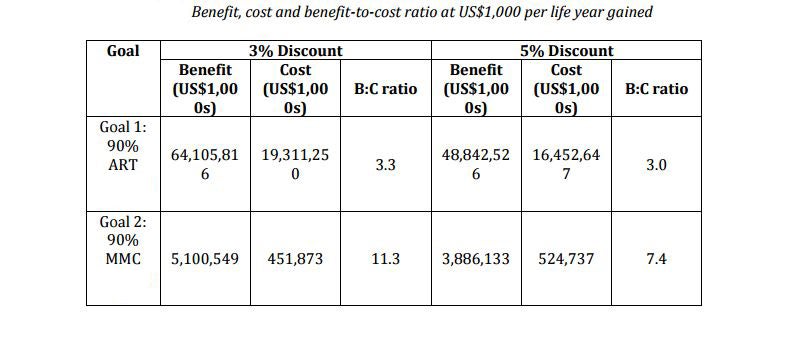
“In the past decade, we have made great strides in pushing back HIV-related deaths and new infections through ART, but we have failed to achieve very high circumcision rates in the HIV-hyperendemic countries in sub-Saharan Africa,” said Bärnighausen.
He believes that adding circumcision campaigns should be an attractive option for countries and donors because it is a one-off procedure that has a lifetime benefit. Bärnighausen explained that achieving large increases in circumcision coverage would require substantial initial funding to cover most uninfected men who are still not circumcised, but that costs would then decline. “Following this initial investment, the maintenance costs to ensure that newborns boys have access to circumcision would be relatively low,” said Bärnighausen, who compared this combination of short-term, large-scale national campaigns and low-level maintenance to past efforts to achieve high coverage with essential childhood vaccines.